
Objectives: To determine the incidence of term breech delivery and to study the influence of mode of delivery on perinatal outcome in pregnancies presenting as breech.Breech Delivery at Term: Do the Perinatal
Results Justify a Trial of Labor?Abdulaziz Al-Mulhim, MBBC, LM*
Turki G Gasim**
Methods: Three hundred and thirty two normal live-born singleton term breech births between 1st January 1996 and 31st December 2000, were studied retrospectively. Fifty eight percent of the patients had vaginal breech delivery, while 42 % were delivered by cesarean sections. The age of the patient, parity, period of gestation, antenatal care, mode of delivery, type of anesthesia, infant birth weight, Apgar score, birth complications and neonatal outcome were recorded in the two groups. Seven patients with intrauterine fetal deaths and lethal congenital fetal anomalies were excluded from the study.
Results: The incidence of breech presentation at term was 2.4%. Forty-nine (14.8%) patients with breech presentation were delivered by elective cesarean section. Two hundred and eighty three patients were subjected to a trial of vaginal delivery, of whom 67.8 % had vaginal breech delivery while 32.2 % were delivered by emergency cesarean section. Slow progress during labor was the most common reason for emergency cesarean section. The patients with footling breech presentation, fetuses with extended head, macrosomic infants and cases of contracted maternal pelvis underwent cesarean section. No statistical difference were found in the neonatal outcome namely Apgar score and admission to NICU between the patients delivered by cesarean section and vaginal birth groups. The neonatal mortality rate was zero in both groups. Increasing maternal age and increasing infants birth weight positively correlated with an increasing rate of cesarean section.
Conclusion: We believe that safe vaginal breech delivery can be achieved in 58% of carefully selected cases without major adverse perinatal outcome.
Bahrain Med Bull 2002;24(1):23-27.
Approximately 3% of all term deliveries are breech presentations1. The optimal mode of delivery of such infants remains controversial2. Vaginal delivery in breech presentation entails high risks of serious complications namely cord prolapse, aspiration of amniotic fluid, maternal and fetal complications associated with the birth process and an increased incidence of operative delivery3.
In order to reduce the mortality and morbidity for infants delivered as breech, liberal use of cesarean section has been recommended3,4. These recommendations caused an increase in cesarean delivery rates5. However, since then, there have been numerous studies reporting contradictory results with regard to the optimal mode of delivery of infants presenting as breech5-9. A critical review of the literature published between 1966 and 1992 suggested that vaginal delivery for term infants in breech presentation was associated with three to four times higher rates of perinatal morbidity and mortality compared to elective cesarean delivery2.
Hannah et al10 in a randomized multicenter trial reported that planned cesarean section was better than planned vaginal birth for the term breech fetuses. On the other hand, many other studies have reported vaginal delivery of the term breech as an acceptable obstetric choice in selected cases6,7,9.
The aim of this study was to determine the incidence of term breech delivery and to study the influence of mode of delivery on perinatal outcome in pregnancies presenting as breech.
METHODS
This was a retrospective study carried out at King Fahad Hospital, Al-Khobar. The hospital receives booked cases from the Obstetrics and Gynecology clinics, emergency admissions, and referred cases from other hospitals and health centers as it is the only tertiary center in the eastern province of Saudi Arabia.
Three hundred and thirty two normal live born singleton term (after 37 completed gestational weeks) infants delivered as breech between 1st January 1996 and 31st December 2000, were included in the study. The medical records of these cases were studied, and the variables namely age of the patient, parity, period of gestation, antenatal care, mode of delivery, type of anesthesia, infant birth weight, Apgar score, birth complications and neonatal outcome were recorded.
Maternal age was defined as completed years at delivery. Parity was defined as number of previous births of gestational age of more than 24 completed weeks (including stillbirths). Estimation of gestational age was based on LMP (Last Menstrual Period) and/or routine ultrasound examinations before the completion of 20 gestational weeks. Regular antenatal care was defined as four visits or more in the obstetric clinics. Mode of delivery was defined as either elective or emergency cesarean or vaginal delivery. Elective cesarean delivery was defined as a cesarean delivery before the onset of labor, and emergency cesarean delivery was defined as one performed after the onset of labor. The breech delivery was conducted by experienced residents. The pediatrician and anesthesiologist were present at the time of delivery.
In the study group, 32.3% of the patients had regular antenatal care in our hospital, 62.4% had some care in the health centers and / or other hospitals, and 5.3% had no antenatal care. As the majority of our patients were unbooked cases, the decision regarding the mode of delivery was made on admission by the experienced senior resident in consultation with senior registrar or consultant.
Breech extraction is not generally employed in our hospital. However, during the study period we used breech extraction in one case because of severe fetal distress in the second stage of labor and the late attendance of patient to the hospital.
Epidural anesthesia was used in approximately 18 % of cases. In others, pudendal block and local perineal infiltration was used. The majority of the cesarean sections were performed under general anesthesia.
Seven patients with intrauterine fetal death and lethal congenital abnormalities diagnosed antenatally were excluded from the study.
In this hospital routine cesarean section for all cases of term singleton breech is not the policy and vaginal delivery in selected cases is an acceptable choice. The decision regarding the mode of delivery was made on the basis of estimated fetal weight, type of breech presentation, attitude of the after coming fetal head and adequacy of the maternal pelvis. The reaction of the patient and her wish regarding the mode of delivery was also taken into account.
The patients were allowed to have a trial of vaginal breech delivery provided there was no contraindication to vaginal delivery. The presentation should be either frank (hips flexed, knees extended) or complete (hips flexed, knees flexed but feet not below the fetal buttocks) without extended head. The estimated birth weight of the fetus should be less than 3500 grams. Clinical assessment of the adequacy of the pelvis was sufficient and pelvimetry was not used routinely in all cases. A trial of labor was only precluded in the presence of medical or obstetric complications.
Soon after the admission, abdominal and vaginal examinations were carried out by an experienced obstetrician in order to assess the size, position and presentation of the fetus, cervical dilatation, status of the membrane and adequacy of the maternal pelvis. Ultrasonic assessment of the fetus was done to determine the gestational age, site of the placenta, estimated fetal weight as well as the type of breech including the presence of a hyper-extended neck. The amount of liquor was assessed and major fetal congenital anomalies were excluded. The laboring patients had continuous electronic fetal monitoring.
Patients with one previous lower segment cesarean were allowed to labor provided they met the criteria of the trial of vaginal delivery.
In this study, the statistical analyses were performed using the Mann-Whitney and chi-square tests wherever appropriate comparing data from the two groups. The difference was considered statistically significant when p £ 0.05.
RESULTS
The total number of deliveries during the study period were 13560. The total number of singleton term breech births included in the study were 332 and this represented nearly 2.4 % of the total deliveries. In the study group, 192 (57.8%) had vaginal breech delivery and 140 (42.2%) had cesarean delivery. Of cesarean delivery 49 ( 14.8 % ) patients underwent elective cesarean section, while 91 (27.4%) were delivered by emergency cesarean sections.
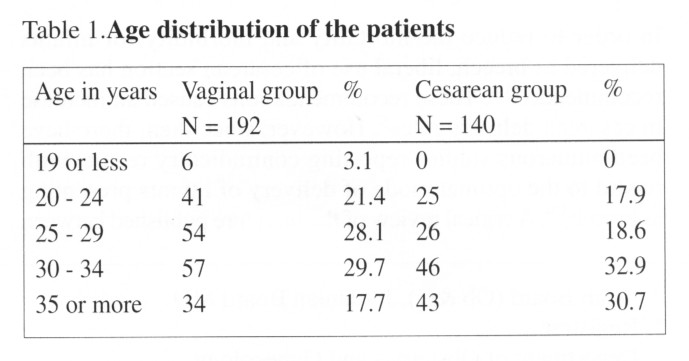
Table 1 shows the age distribution of the patients. The mean age of the patients who had vaginal delivery was 29.1 ± 6 years ( SD ), while those who underwent cesarean was 33.8 ± 6.3 years ( SD ). The difference was statistically significant ( p < 0.001 ).
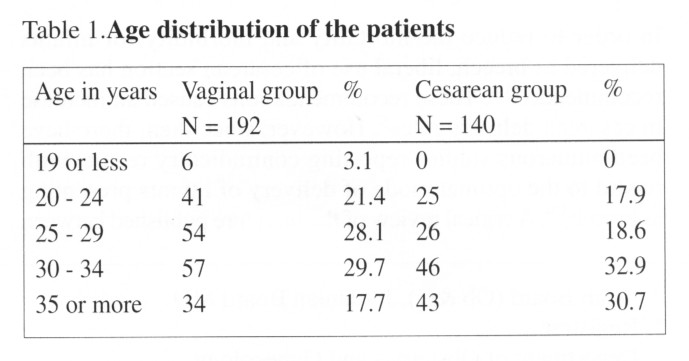
Table 2 shows the parity distribution of the patients. The mean parity of the patients who had vaginal breech delivery was 3.2 ± 2.8 (SD), while those who underwent cesarean was 3.2 ± 2.9 (SD). The difference was statistically insignificant.
The mean gestational age of the patients who had vaginal breech delivery was 39.5 ± 1.2 weeks (SD), while those who underwent cesarean was 39.4 ± 1.4 weeks (SD). The difference was statistically insignificant.
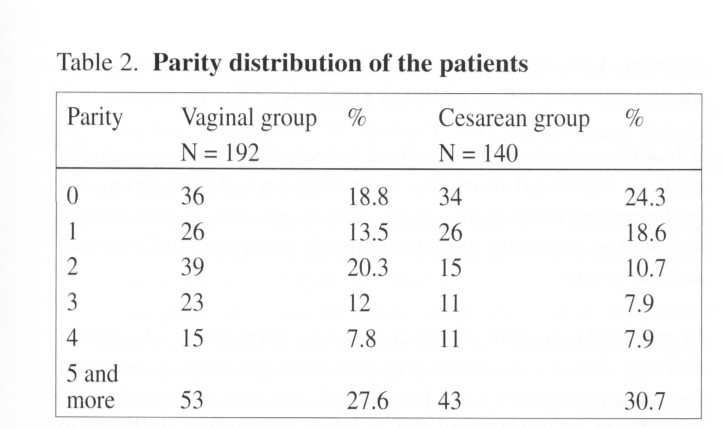
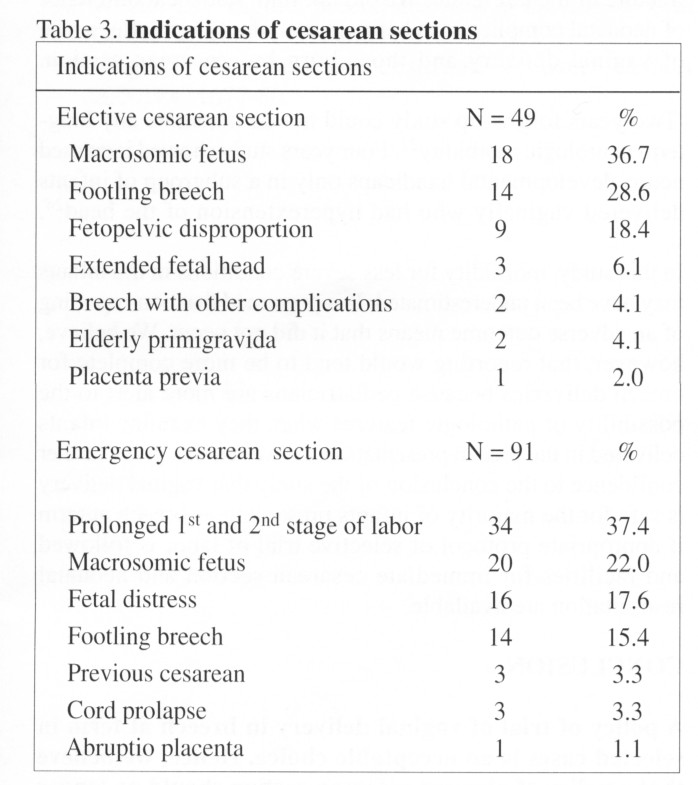
Table 3 lists the indications of elective and emergency cesarean sections. Slow progress during labor was the commonest indication of emergency cesarean section. Thirty eight (27.1%) cesarean sections were performed because of macrosomic infants, 20 (14.3%) of these infants were of diabetic mothers. Ten patients had one previous cesarean section due to causes other than fetopelvic disproportion, they fulfilled the criteria for trial of vaginal delivery. Three (30%) of the 10 cases ended by cesarean section due to failure to progress, while the remaining 7 (70%) had a successful vaginal delivery.
Emergency cesarean section N = 91 %
Prolonged 1st and 2nd stage
of labor 34 37.4
Macrosomic fetus
20 22.0
Fetal distress 16 17.6
Footling breech 14 15.4
Previous cesarean
3 3.3
Cord prolapse 3 3.3
Abruptio placenta 1 1.1
Table 4 summarizes the infants birth weight distribution. The mean birth weight of the infants delivered vaginally was 3006 ± 471 grams (SD), while of those delivered by cesarean section was 3570 ± 716 grams (SD). The difference was statistically significant (P < 0.0001).
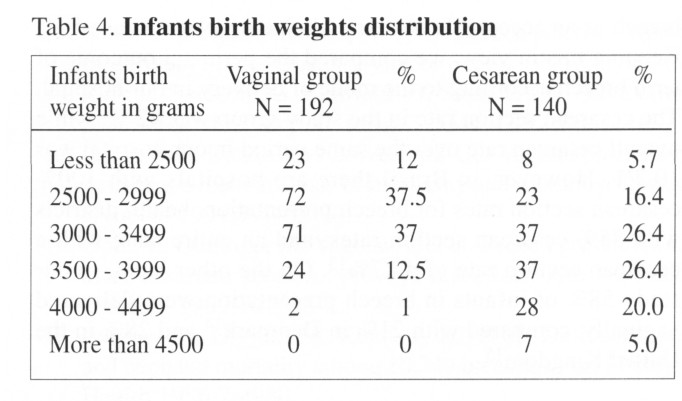
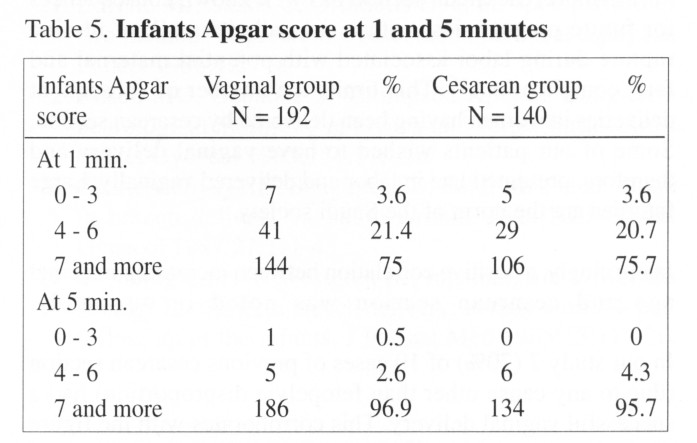
Table 5 shows the Apgar score of infants at one and five minutes. Twenty five percent of the infants in the vaginal birth group had Apgar score less than 7 at one minute as compared to 24 % of the infants delivered by cesarean section. The difference was statistically insignificant. Furthermore, 6 (3.1%) infants in the vaginally delivered group and 6 (4.3%) in the cesarean delivered group had Apgar score less than 7 at 5 minutes.
One patient had postpartum hemorrhage due to cervical laceration and this patient had breech extraction. Five cases of wound infection were seen in cesarean section group.
The number of infants requiring admission to nursery intensive care unit was 5 (2.6%) for the vaginal deliveries, and 4 (4.4%) for the cesarean deliveries. The difference was statistically insignificant. One infant in the vaginally delivered group had fracture of the left femur as a result of breech extraction, which was carried out because of severe fetal distress in the second stage of labor. This patient was a primigravida presented to the hospital late in labor. The birth weight of the infant was 3380 gram and the Apgar score was 6 and 10 at 1 and 5 minutes respectively. The infant was admitted to nursery intensive care unit for 4 days for observation and discharged along with the mother 6 days postpartum with a splint. He was given a follow up appointment to attend the Paediatric orthopedic clinic. There were no intrapartum or neonatal deaths recorded during the study period.
DISCUSSION
The incidence of breech presentation at term in
this study was 2.4%. This corroborates with the figures reported in other
studies1,11. The management of breech presentation at term
has remained controversial and some authors recommend a policy of elective
cesarean section for all term breech fetuses4,6,12. This
has led to an increased use of cesarean section. Recently, a number of
studies have reported vaginal delivery of the term breech as an acceptable
obstetric choice in selected cases6,7,9. Keeping this in view,
we compared the perinatal outcome of term breech according to the mode
of delivery in our hospital. The cesarean section rate in the study group
was 42 %, while overall cesarean rate over the same period in our hospital
was 10.7%. However, in Brazil there are hospitals with 100% cesarean section
rates for breech presentation, health districts with 85% cesarean section
rates, and an entire state with a cesarean section rate of 47·7%13.
On the other hand, in our study 58% of infants in breech presentation were
delivered vaginally, compared with 21% in Denmark14 and 28% in the United
Kingdom15.
Cesarean section is a major surgical procedure
and maternal morbidity has been shown to be higher after a cesarean delivery
in comparison to a vaginal birth6. In addition, delivering
women by caesarean section results in a significantly longer hospital stay.
In this study the average length of the hospital stay of the patients having
had cesarean section was 6 days, while vaginally delivered patients were
generally discharged after 12 days. Furthermore, caesarean section has
well known consequences for future pregnancies, with a risk, albeit small,
of uterine rupture during labor associated with potential maternal and
fetal complications16. This limits the number of subsequent
deliveries in women having been delivered by cesarean section. Some of
our patients wished to have vaginal delivery and therefore, presented late
in labor and delivered vaginally. Large families are the norm of the Saudi
society.
Interestingly, a positive correlation between
increasing maternal age and cesarean section was noted in our study.
In our study 7 (70%) of 10 cases of previous cesarean section (due to any cause other than fetopelvic disproportion) had a successful vaginal delivery. This corroborates with the figure reported by Ophir et al17. They offered 66% of the patients with one previous cesarean section a trial of labor, of whom 79% delivered their breech infants vaginally.
In our study the mean birth weight of the term breech infants delivered by cesarean section was significantly higher than those delivered vaginally. The management of large breech infants remains controversial. For vaginal delivery it has been stated that perinatal morbidity and mortality increase with birth weight14,18. Investigators have suggested different limits for birth weight, above which elective cesarean section is indicated, such as 3500 gm14, 4000 gm19, and 4500 gm6. We feel justified to maintain a weight limit at 3500 gm for vaginal delivery when conditions are otherwise considered optimal. In our study, the mean birth weight of the vaginal group was 3.0 kg, while that of the cesarean section group was 3.6 kg.
The Apgar score is widely used as an index of the severity of intrapartum asphyxia. However, the Apgar score is a nonspecific description of vitality at a particular time and a poor predictor of later sequelae unless a low Apgar is maintained beyond 5 to 10 minutes20 or is accompanied by significant hypoxic ischemic encephalopathy during the days after birth20,21. Although an Apgar score less than 7 at 1 minute was observed almost equally in the group delivered vaginally and by cesarean section, not all these infants needed admission to the neonatal intensive care unit and none had severe signs of encephalopathy in the neonatal period. Breech vaginal delivery may be associated with a higher risk of depression at birth but not with later sequelae if the deliveries are carefully conducted and appropriate management of the newborn is available20,21.
It has been claimed that vaginal breech delivery
is associated with an increased mortality from intracranial hemorrhage22.
In the current study there was no case of intracranial hemorrhage in both
the vaginally delivered breech group and the cesarean section group.
In our study, inspite of the increasing proportion
of vaginal delivery and the decreasing use of cesarean section, no trend
toward an increased need for special care was observed. This is in
favor of continuing the practice of vaginal delivery in properly selected
cases. The overall corrected perinatal mortality rate in our hospital was
15/1000 live births over the study period, while for the breech deliveries
the corrected perinatal mortality was zero. Chattopadhyay et al from Riyadh,
reported 19% cesarean rate in term breech deliveries, and the overall corrected
perinatal mortality rate in their study was 36/1000 live births, while
18/1000 live births for breech23.
The risk of neonatal death attributable to vaginal breech delivery has been calculated by various authors to be about 4 per 100015. The current study could not confirm this because the corrected neonatal mortality was zero.
Trauma associated with vaginal delivery in breech
presentation did not represent a major problem although one infant had
fracture of the left femur. We did not find statistical difference
of neonatal complications between the infants born after a trial of vaginal
delivery and those born by cesarean section.
Two years follow-up study could not demonstrate
any long-term neurologic morbidity 22. Four years study showed
increased neuro-developmental handicaps only in a subgroup of infants delivered
vaginally who had hyperextension of the head24.
In this study, morbidity for less severe conditions in the infants may have been underestimated. It is presumed that non-reporting of an adverse outcome means that it did not occur. We believe, however, that reporting would tend to be more complete for breech deliveries because pediatricians are more alert to the possibility of pathologic features when they examine infants delivered in the breech presentation. However, this gives further confidence to the conclusion of the study that vaginal delivery is safe for the majority of infants presenting as breech at term if appropriate protocol of selective trial of labor is followed and facilities for immediate cesarean section and neonatal resuscitation are available.
CONCLUSION
A policy of trial of vaginal delivery in breech at term in selected cases is an acceptable choice. Hence, we believe that a policy of planned cesarean section should no longer be encouraged as being the sole method of delivery in breech presentation at term.
REFERENCES
1. Stiff E, Friedman S, Mashiach S, et al.
Maternal and neonatal outcome of
946 singleton breech
deliveries. Am J Obstet Gynecol 1996;175:18-23.
2. Cheng M, Hannah M. Breech delivery at term:
A critical review of the
literature. Obstet
Gynecol 1993;82:605-18.
3. Fischer - Rasmussen W, Trolle D. Abdominal
versus vaginal delivery in
breech presentation.
Acta Obstet Gynecol Scand 1967;9:69-76.
4. Wright RC. Reduction of perinatal mortality
and morbidity in breech
delivery through
routine use of cesarean section. Obstet Gynecol
1959;14:75863.
5. Croughan-Minihane M, Petitti D, Gordis L,
et al. Morbidity among breech
infants according
to method of delivery. Obstet Gynecol 1990;75: 821-5.
6. Collea JV, Chein C, Quilligan EJ. The randomized
management of term frank breech presentation at term: A study of 208 cases.
Am J Obstet Gynecol 1980;137:235-49.
7. Myers S, GleicheTN. Breech delivery: Why the
dilemma? Am J Obstet
Gynecol 1986;155:
6-10.
8. Erkkola R. Controversies : Selective vaginal
delivery for breech
presentation.
J Perinat Med 1996;24:553-61.
9. Rosen M, Chik L. The effect of delivery route
on outcome in breech
presentation.
Am J Obstet Gynecol 1984;148:90914.
10. Hannah ME, Hannah WJ, Hewson SA, et
al. Planned cesarean section
versus planned
vaginal birth for breech presentation at term : a randomized
multicenter trail.
Lancet 2000;356:1375-83.
11. Hickok DE, Gordon DC, Milberg JA, et
al. The frequency of breech
presentation
by gestational age at birth : a large population-based study.
Am J Obstet
Gynecol 1992;166:85152.
12. Weiner CP. Vaginal breech delivery
in the 1990s. Clin Obstet Gynecol
1992;35:55961.
13. Wagner M. Choosing cesarean section. Lancet
2000;356:167780.
14. Krebs L, Langhoff-Roos J, Weber T. Breech
at term - Mode of delivery?
Acta Obstet Gynecol
Scand 1995;74:7026.
15. Thorpe-Beeston JG, Banfield PJ, Saunders
NJ. Outcome of breech delivery
at term.
BMJ 1992;305:746-7.
16. Rosen MG, Dickinson JC, Westhoff CL. Vaginal
birth after cesarean; a
meta-analysis
of morbidity and mortality. Obstet Gynecol 1991;77:465-70.
17.Ophir E, Oettinger M, Yagoda A, et al. Breech
presentation after cesarean
section : Always
a section? Am J Obstet Gynecol 1989;161: 25-8.
18. Fortney JA, Higgins JE, Kennedy KI, et al.
Delivery type and neonatal
mortality among
10,749 breeches. Am J Public Health 1986;76:980.
19. Songane FF, Thobani S, Malik H, et al.
Balancing the risks of planned
cesarean section
and trial of vaginal delivery for the mature, selected,
singleton breech
presentation. J Perinat Med 1987;15:531-43.
20. Nelson KB, Leviton A. How much of neonatal
encephalopathy is due to
birth asphyxia.
Arch Pediatr Adolesc Med 1991;145:132531.
21. Levene MI, Sands C, Grindulis H, et al.
Comparison of two methods of
predicting outcome
in perinatal asphyxia. Lancet 1986;1:679.
22. Rosen MG, Debanne S, Thompson K, et al. Long-term
neurological
morbidity in breech
and vertex births. Am J Obstet Gynecol
1985;151:71820.
23. Chattopadhyay SK, Sengupta BS, Zaidi MH,
et al. Trend in breech delivery
in Saudi Arabia.
Aust NZJ Obstet Gynecol 1987;27:111-4.
24. Svenningsen NW, Westgren M, Ingemarsson I.
Modern strategy for the
term breech delivery:
a study with a 4-year follow-up of the infants. J
Perinat Med 1985;13:11726.
------------------------------------------------------------------------------------
*Arab Board (Ob &G), Jordanian Board
MD
**Registrar
Department of Obstetrics and
Gynecology
King Fahd Hospital of the
University
Al-Khobar, Saudi Arabia
Copyright 2001, Bahrain Medical Bulletin