Very Low Birth Weight and Extremely
Premature Babies at KAUH
Haifa A Mansouri, FRCSC*
Aim: The study was conducted at King Abdulaziz University Hospital (KAUH) over ten years period to evaluate the neonatal mortality and morbidity of very low birth weight (VLBW) and very preterm infants and to look at the incidence of cerebral palsy in the surviving infants.
Methods: A retrospective chart review of mother and babies with VLBW (³ 500 gms and £ 1500 gms) and a gestational age <32 weeks delivered at KAUH between August 1996 to the end of July 1996 was done. The review looked at maternal characteristics and complications during pregnancy, neonatal mortality and morbidity and follow up of surviving infants. A comparison was made between those born with a gestational age of 22-26 weeks (group A) and 27-31 weeks (group B).
Results: Ninety-two VLBW were evaluated. The incidence of VLBW babies at KAUH was 0.52%. The neonatal mortality was 23.8% while the early neonatal mortality was 22.8%. There was no significant difference in maternal characteristics and complications between the two groups A & B. The early neonatal mortality of group A (75%) was significantly higher than group B (13.7%), while the immediate neonatal complications including hyperbilirubinemia, respiratory distress syndrome (RDS), neonatal sepsis, electrotype and pH disturbances were significantly higher for group B babies than group A.
Bronchopulmonary dysplasia (BPD) and intraventricular haemorrhage (IVH) were not significantly different between the 2 groups. Among 64 survivors, thirty were followed for at least 12 months and of these, 7 infants (23.33%) had cerebral palsy (CP) and two (4%) had minor deficits.
Conclusion: VLBW and very premature babies are a major cause of neonatal mortality and morbidity. The incidence of cerebral palsy and minor deficits at our institution is comparable to that quoted in other literature.
Bahrain Med Bull 2001;23(2):66-70
Very preterm delivery of women with associated VLBW (< 1500 grams) of their infants is a major perinatal problem with increased neonatal morbidity and mortality. Very preterm births account for preterm infants for almost half the total perinatal mortality and 80% of neonatal deaths are in preterm infants1,3
Post-natal growth and development of VLBW infants (birth weight < 1500 grams) has been the subject of many studies conducted in developed countries. However, these data can not readily be extrapolated to be used for developing countries because of major differences in the availability and level of intensive care facilities and the differences in demographic and socio-economic conditions which are likely to affect both pre-natal and post-natal growth and development4.
In present times, 85% of the infants born with birth weight less than 1500 grams (VLBW) will survive without handicap1,2,5. Nevertheless, infants surviving a birth weight < 1500 gms are a hundred times more likely to have disabling cerebral palsy than infants of the most common birth weight group, 3000 to 3500 gms6.
This study was conducted to evaluate the outcome of VLBW and very preterm infants and the follow up of the surviving infants over ten years at KAUH.
METHODS
The data of this study was collected from the medical records of all VLBW infants delivered at King Abdulaziz University Hospital between August 1986 to the end of July 1996. Both the mother’s and baby’s records were reviewed. All babies with a birth weight > 500 gms and less than 1500 gm, either singleton or multiple pregnancies, and less than 32 weeks gestational age were included in the study. VLBW babies delivered in other hospitals and admitted to our Noenatal Intensive Care Unit (NICU) were not included.
The study looked at the maternal characteristics and neonatal factors of 2 groups of VLBW babies, those born with a gestational age of 22 – 26 weeks (group A), and those between 27 – 31 weeks (group B).
The maternal characteristics included were: age; parity; a history of previous preterm delivery, a history of previous low birth weight or a history of previous neonatal death; number of antenatal visits and maternal complications including: pregnancy induced hypertension (PIH), diabetes, anemia, antepartum haemorrhage, preterm labour and premature rupture of membranes (PROM). The gestational age at delivery and the date and mode of delivery were also recorded. The gestational age at delivery was determined by date of last menstrual period and ultrasound examination whenever it was available and this was confirmed by pediatric assessment following delivery.
The neonatal parameters looked for, included: birth weight, length, head circumference, Apgar score at 1, 5 and 10 minutes (cord gases are not done in this institute), number of days the neonate was ventilated and the number of days of NICU and hospital admission.
The neonatal complications included were: hyperbilirubinemia, respiratory distress syndrome and if surfactant was used, neonatal sepsis (diagnosed clinically or confirmed with cultures with proven necrotising enterocolitis or meningitis etc), neonatal convulsions, electrolyte disturbances and/or metabolic acidosis. Birth asphyxia was diagnosed by the pediatricians’ if there was low Apgar score<7 at 5 and 10 minutes with associated metabolic acidosis, convulsions and or multi-system organ involvement.
The presence of intraventricular haemorrhage was diagnosed clinically and confirmed by ultrasound (not being done as routine for VLBW in this institute). Broncho pulmonary dysplasia was diagnosed if the neonate required > 28 days of assisted ventilation.
All babies discharged were given appointments for follow-up. Those who attended were assessed regularly and routinely every 3 months by a Paediatrician. The presence of minor disabilities were noted. Cerebral palsy was diagnosed by the Paediatrician according to standard criteria, at least after 1 year of follow-up.
Babies of gestational age 22 – 26 weeks were compared with those of 27 – 31 weeks gestational age in relation to perinatal factors, maternal characteristics, neonatal and long term complications.
RESULTS
One hundred and thirty three VLBW babies were born at KAUH. One hundred and thirty one charts were available for review. Of these, thirty nine were excluded because they were VLBW but with a gestational age > 32 weeks. Ninety-two cases were evaluated for both maternal and neonatal characteristics.
The total number of live births at KAUH was 25, 753 births over the ten years period. Of these, 1,716 births were LBW (6.7%) and 133 VLBW (0.52%). Only 23 VLBW neonates were part of multiple pregnancy. The details are shown in Table 1.

Of the ninety-two evaluated cases, twenty one (22.8%) died as early neonatal deaths (ENND) and one as late neonatal death (LNND). The neonatal mortality rate was 23.9%. Two babies died at the age of 30 and 34 days. Of the surviving infants, sixteen of the children were lost to follow up while 50 were followed up for a period of 2 – 120 months. Of those followed, 30 were followed for more than one year.
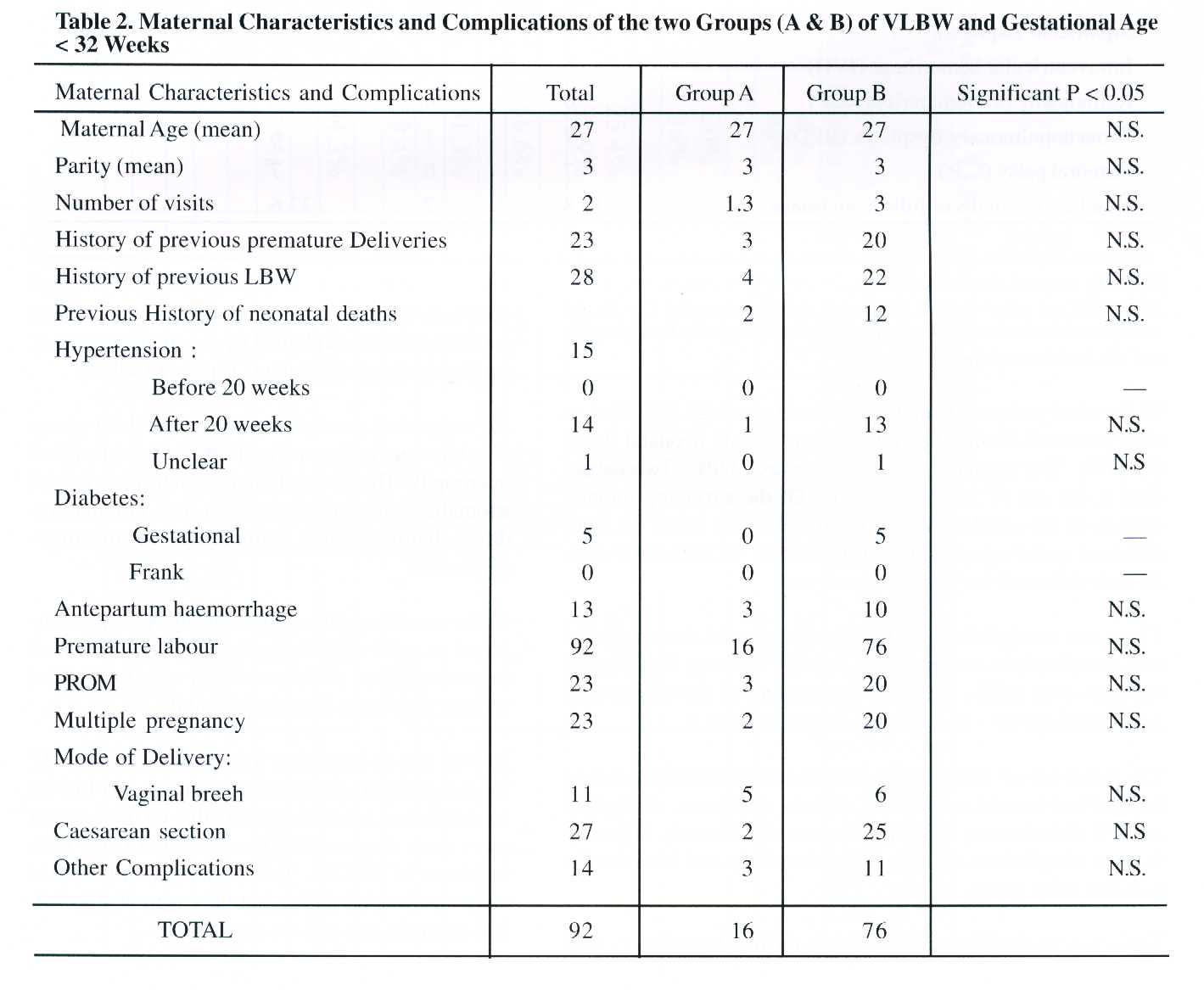
There was no significant difference in maternal
characteristics and complications and mode of delivery between 2 groups
of neonates born at 22 - 26 weeks as compared to those born with gestational
age 27 – 31 weeks as shown in Table 2.
The early neonatal death rate was significantly higher (75%) in the lower gestational age group than the higher gestational age group (13.7%) and as expected the birth weight was significantly lower in the first group A, and this is shown on Table 3.

The incidence of immediate neonatal complications including hyperbilirubinemia, respiratory distress syndrome, electrolyte and PH disturbances and asphyxia was significantly higher in the surviving infants, of higher gestational age and birth weight than the other group.
There was no significant difference in the number of cases with intraventricular haemorrhage (IVH) and bronchopulmonary dysplasia (BPD) between the two groups and this could be explained by the small number of survivors of group A infants (only 4) Table 3.
No congenital anomalies were reported for group A, while 6 major anomalies (7.9%) were identified in group B. These were Potter’s syndrome, skeletal anomalies with lung hypoplasia, non-immune hydrops, hydrocephalus , exomphalus and meningomyelocele.
Of the surviving infants from group A, 2 were followed to age 9 and 11 months with no evidence of any neurological deficits and two were lost follow up after discharge from the hospital.
Among the 64-surviving infants from the 27 – 31
weeks (group B) gestational age group, 30 (46.9%) were followed for at
least 12 months. Of these, seven cases were diagnosed to have cerebral
palsy with incidence of 23.33%. Two neonates (4%) had minor sensorineural
deficit but they were lost to follow-up at the age of 4 – 6 months.
DISCUSSION
The literature varied regarding the outcome of VLBW infants, with the new trend towards mainly assessing the outcome of extremely low gestational age < 28 or very preterm infants.
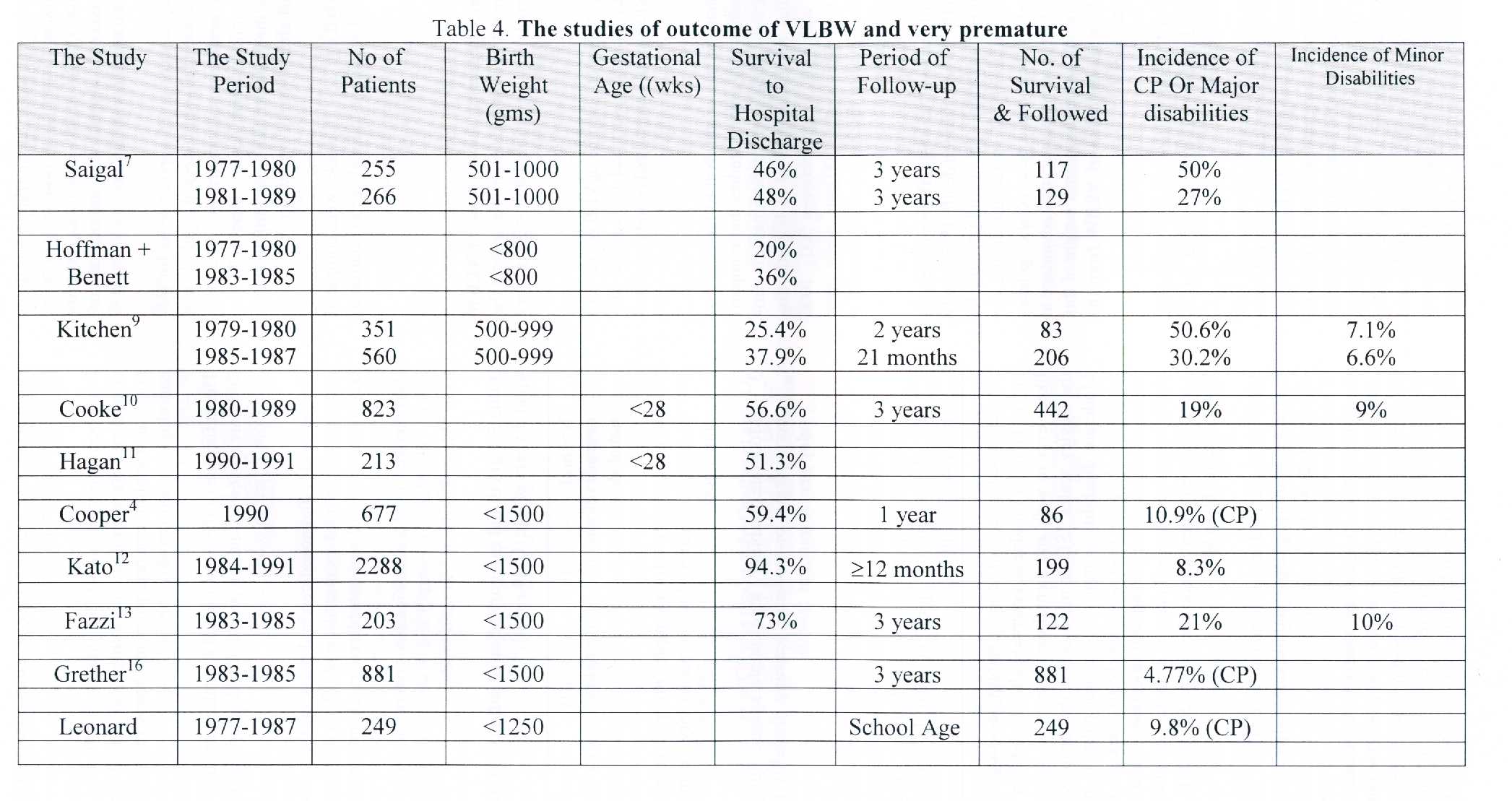
Table 4 shows the studies of outcome of VLBW and very premature infants including survival to hospital discharge and the incidence of cerebral palsy and major and minor disabilities.
It will be noted that the rate of survival to hospital discharge varied considerably among studies, but comparison could not be easily made, as the denominator is variable. Some studies reviewed survival to hospital discharge of babies with birth weight between 500 – 1000 gms, others used birth weight of <1500 gms, while some authors reviewed survival to discharge of babies with a gestational age <28 weeks.
The highest rate of survival to hospital discharge was reported by Kato et al12 where thirteen deaths (5.5%) only occurred during hospitalization. This could possibly be explained by the availability of surfactant during the whole study period, or there could be a racial or genetic factor of Japanese babies to have a survival advantage at a lower birth weight and or the mean birth weight of this race is lower and so the deviation of VLBW from the mean is not as great.
In our study of 92 VLBW and gestational age <32 weeks, 66 (73.9%) survived to hospital discharge and this is comparable to other studies.
It will be observed that the incidence of maternal complications associated with this group of VLBW babies is higher than in the general pregnant women. Premature rupture of the membranes (PROM) was a significant cause of prematurity in this group (25%). The incidence of antepartum haemorrhage leading to premature delivery was 14.1%, while hypertension occurred in 16.3% and gestational diabetes in 5.4% of the patients. Other complications included sickle cell anaemia, bronchial asthma, cervical cerclage etc, and these accounted for 14.4% of the cases shown in Table 2.
It has been reported that VLBW infants <1500 grms are at high risk for neurologic disability. One in 20 survivors has disabling cerebral palsy and many others have neurologic or sensory difficulties14.
The definition of the neurological sequalae varied in the literature reviewed and the period of follow up was variable from 1 year to school age.
Cooper et al14, diagnosed cerebral palsy on the basis of neurodevelopmental examination at 12 months and a Bayley score of <70 was considered as a handicap.
RWI Cooke10 used a classification system shown in Table 5. The infants in group 3 and 4 were considered to have “Major Disability” in their study.

Kitchen9 used criteria of severe disability as comprising any of bilateral blindness, cerebral palsy in children unlikely ever to walk and mental developmental index on the Bayley scales 2SD or more below the mean (<69). Moderate disability comprised cerebral palsy in non-ambulant children who were likely to walk or sensorineural deafness requiring amplification. Mild disability comprised cerebral palsy in ambulant children or a mental developmental index between 1SD to 2SD below the mean (69 to 84).
Kato12 et al, defined major handicap as cerebral palsy, mental retardation, epilepsy and blindness after a period of 1 year follow up.
Grether et al16, defined cerebral palsy as a chronic disability of central nervous system origin characterized by aberrant control of movement or posture, appearing early in life and not the result of progressive disease. Excluded were children whose cerebral palsy was acquired through an adverse event after the first 28 days life or a disability as a result of meningomyelocele or solely caused by mental deficiency or isolated hypotonia.
Fazzi et al13, have used Amid-Tison and Grenior neurological access and Bayley scales of infants development categories included minor sequale: tone and reflex anomalies DQ/IQ 71 – 84, Strabismus or mild myopia, or ventricular-peritoneal shunts in subjects with normal development. Major sequale in any form of cerebral palsy, DQ / IQ < 70 hypoacusis needing a device, mono or bilateral blindness to retrolental fibroplasia or multiple minor sequale.
Synnes et al17, defined major impairments as motor impairment compatible with a clinical diagnosis of cerebral palsy on neurologic examination visual impairment with refractive correction worse than 20/2000, auditory impairment requiring amplification and intellectual impairment with a score less than – 2SD on the mental development index (Bayley scales).
Leonard et al15, diagnosed cerebral palsy on the basis of neuro-developmental examination at 1 year and at school age.
In our study cerebral palsy was diagnosed on the basis neurodevelopmental examination at 12 months. No cases of blindness due to retinopathy of prematurity (ROP) has been diagnosed although there were 6 cases with ROP but these were not severe to cause blindness. Severe hearing loss was not diagnosed in any infants
The lowest rate of CP was reported by Grether et al16. Of 881 singleton children if VLBW < 1500 gms and survived to the age of 3 years; 42 (4.77%)had moderate or severe congenital C.P. They excluded mild C.P., transient motor abnormalities or disability as a result of meningomyelocele or solely caused by mental deficiency and isolated hypotonia.
It is obvious when looking at the above data, that the results are not easily compared as some have used VLBW outcomes and others have used outcomes related to gestational age and even when VLBW was used different birth weight groups all < 1500 but varied between 500 – 999 gms to < 1250 gms.
The period of follow-up among studies also varied from 1 year to school age, but most important is that when the number of cerebral palsy cases was related to all alive births and then showed the lowest rate, while others related it to number of survivors and those were the highest rates.
When these considerations were taken into account, the rate of CP from our study is comparable to others.
CONCLUSION
Very low birth weight and extremely premature infants is a major cause of perinatal mortality and disability. The number of cases in our study is small, but it revealed a comparable outcome of VLBW and extremely premature to international reported outcomes. The follow-up of our patients could be improved by educating parents and the public for the importance of early detection of abnormalities and early treatment or rehabilitation. The definitions of the different disabilities should be standardized and the perinatal outcome parameters should be unified for reporting, so comparisons can be done easier. More efforts should be done to decrease the rate of preterm birth and that is usually a central issue in modern obstetrics.
REFERENCES
1. Hoffman HJ, Bakketta LS. Risk factors
associated with the occurrence of preterm birth.
Clin Obstet Gynecol
1989;27:539-552.
2. Kramar MS. Birth weight and infant mortality:
Perceptions and pitfalls. Paediatr Perinata
Epidemiology 1990;4:373-381.
3. Lumley J. Preventing and managing prematurity:
Int J Technol Assess Health Care
1991;7460-477.
4. Peter A, Cooper PA, Sandler DL. Outcome
of very low birth weight infants at 12 to 18
months of age in Soweto,
South Africa. Paediatrics 1997;99:537-4.
5. Weisglas-Kuperus N, Baerts W, Saver
PJJ. Early assessment and neuro-developmental
outcome in very
low birth weight infants. Acta Paediatr 1993;82:449-53.
6. Grether J, Nelson BK. Prenatal and Perinatal
factors and cerebral palsy in VLBW infants J
Paediatr 1996;128:407-14.
7. Saigal S, Roentbaum P, Hatterslety B,
et al. Decreased disability rate among 3 years old
survivors weighing 501
to 1000 grams at birth and born residents of a geographically defined
region from 1981 to
1984 compared with 1997 to 1980. J Pediatr 1989;114:836-46.
8. Hoffman EL, Bennett FC. Birth weight
< 800 g changing outcomes and influences of gender
and gestation number.
Pediatrics 1990;86:27-34.
9. Kitchen WH. The victorian infant collaborative
study group. Improvement of outcome for
infants of birth
weight under 1000 gm. Arch Dis Child 1991;66:765-9.
10. Cook RWL. Factors affecting survival
and outcome at 3 years in extremely preterm infants.
Arch Dis Child
1994;71:F28-F31.
11. Hagan R, Benninger H, Chiffings D, et al.
Very preterm birth – a regional study. Part 2:
The very preterm
infant. Br J Obstet Gynaecol 1996;103:239-245.
12. Kato EH, Yamada H, MatsumotoS et al.
Relationship between perinatal factors and outcome
of VLBW
infants. J Perinat.Med. 1996;24:677-86.
13. Fazzi E, Lanzi G, Gerardo A, et al.
Neuro developmental outcome in VLBW infants with or
without periventricular
haemorrhage and 1 or leuco malacia. Acta Paediatr 1992;81:808-11.
14. Nelson K. Magnesium sulfate and risk of cerebral
palsy in VLBW infants. JAMA
1996;276:22:1843-4.
15. Leonard CH, Piecuch RE, Ballard RA,
et al. Outcome of very low birth weight infants:
Multiple gestation versus
singletons. Pediatrics 1994:93.
16. Grether JK, Nelson K, et al. Prenatal
and perinatal factors and cerebral palsy in very low
birth weight infants.
J Pediatr. 1996;128:407-14.
17. Synnes A, et al. Perinatal outcomes
of a large cohort of extremely low gestational age
infants (twenty-three
to twenty-eight completed weeks of gestation). J Pediatr. 1994;125:952-
60.
--------------------------------------------------------------------------------------------------------
* Consultant & Assistant Professor
Department of Obstetrics & Gynaecology
King Abdulaziz University Hospital
Jeddah, Saudi Arabia

