of Osteomyelitis
Haider Abdul-Lateef Mousa, MBChB, MSc*
Thamer A Hamdan, MBChB, FRCS**
Sundus S Bakr, BSc, PhD***
Objective: To investigate clinical aspects and aetiological agents of osteomyelitis with special emphasis on anaerobic infection.
Setting: Basrah University Teaching Hospital, Iraq.
Design: A prospective study.
Methods : Aerobic and anaerobic cultures were made for all cases. The inoculation of operative material on culture media was performed by the bedside.
Results: The study included 134 patients with osteomyelitis. The cases were divided clinically into 4 main groups: haematogenous, exogenous, postoperative and mastoiditis. Staphylococcus aureus was the most common causative agent in haematogenous osteomyelitis whereas Pseudomonas sp. were the most common causative organisms in postoperative and mastoiditis groups of bone infection. The total number of isolated bacteria was 224, of which 50 (22%) were anaerobes. These anaerobes were isolated from 39 (29%) of 134 patients. The anaerobic organisms were found most frequently in the cases of chronic mastoiditis (57%) and erogenous osteomyelitis (40%).
Conclusion: High prevalence rate of anaerobic bone infection was found specially in chronic cases. Thus, conventional treatment measures may not be beneficial and special type of management should be applied for these cases. Anaerobic culture is also recommended for all cases with osteomyelitis.
Bahrain Med Bull 2001;23(2):61-65.
The route of bone infection of osteomyelitis is of three types: haematogenous, direct inoculation, or postoperative. Pyogenic haematogenous osteomyelitis is the most frequent type in children1. While many types of micro-organisms including viruses and fungi may cause osteomyelitis, it is usually bacterial in origin2.
In developed countries, acute osteomyelitis is uncommon. In developing countries the disease still exists and the morbidity appears worse in the lower socioeconomic groups3. In studies of osteomyelitis, Staphylococcus aureus has continued to be the most common pathogen isolated from patients with infected bone. Aerobic and facultative Gram negative bacteria, however, have emerged as significant pathogens in patients with chronic osteomyelitis, osteomyelitis following injury and osteomyelitis associated with an adjacent septic focus4.
Anaerobic bacteria have received increasing recognition as potential pathogens in a variety of infections, but only few authors have noted their role in osteomyelitis. Anyhow, the incidence of anaerobic osteomyelitis is greater than was previously believed4,5.
However there is a lot of evidence of continuing detection of anaerobic pathogens in osteomyelitis, in particular of those previously considered to have little or no pathogenic significance. Anaerobes became a major problem since they are able to multiply in the devitalized tissue with low oxygen or blood supply specially in the sequestra.
Therefore, this study was performed to investigate the causative agents in different types of osteomyelitis with special reference to anaerobes.
METHOD
This study was conducted at Basrah university teaching hospital starting from 15th November 1992 to the 10th of August 1993. The cases involved in the study were 134 patients with osteomyelitis. The clinical diagnosis of osteomyelitis was supported by radiographs and positive cultures of suitable specimens.
The specimens were taken at the time of operation. The vital point was that, in every case the inoculation of the specimens was done immediately in the operating theater (bedside inoculation) and incubated under aerobic and anaerobic conditions without using transport media. The proper and rapid cultivation method led to good results particularly in isolation of strict anaerobic bacteria.
The following media were employed for the isolation of aerobic bacteria: blood agar, chocolate agar (for incubation under 5-10% C02) and MacConkey's agar. Blood agar, phenyl ethanol agar, bacteroides bile esculin agar and egg yolk agar were used for anaerobic culture. GasPak anaerobic jar (BBL) was used for anaerobic incubation.
RESULTS
The study included 134 cases which were divided clinically into 4 main groups of osteomyelitis: haematogenous, exogenous, postoperative and mastoiditis.
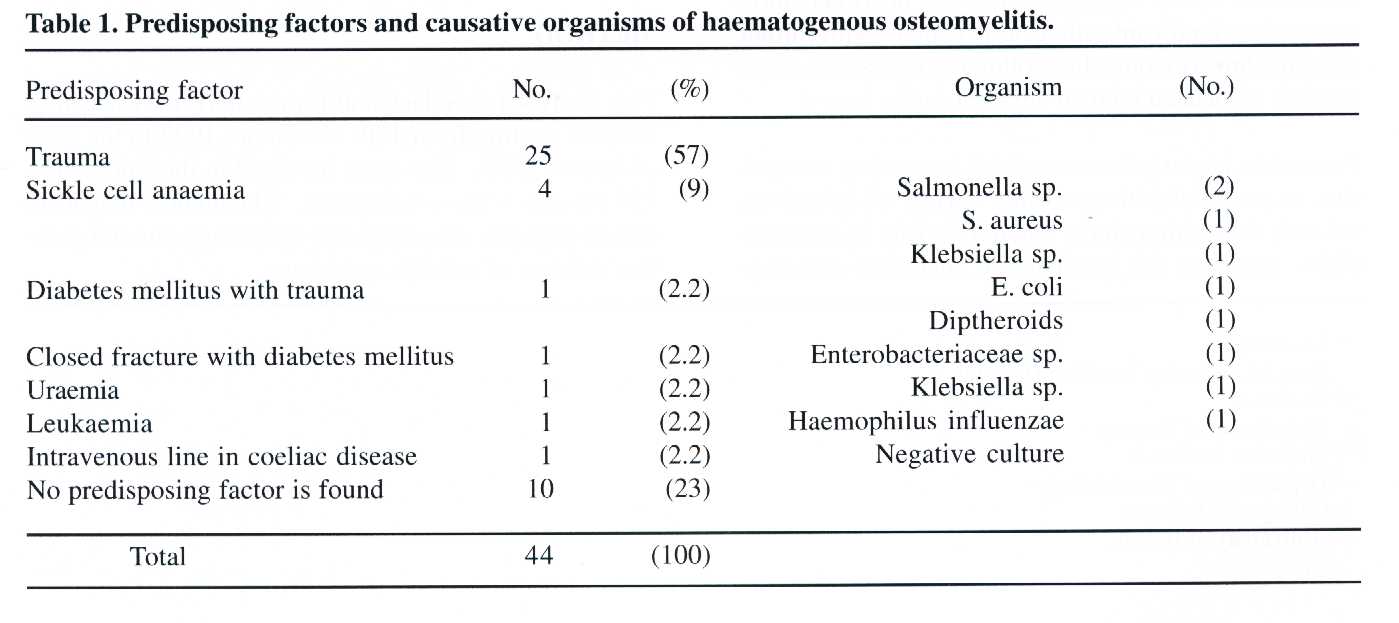
Haematogenous osteomyelitis
There were a total number of 44 cases of which 29 were males and 15 were females. Male to female ratio was 1.9: 1. The age of patients ranged from 3 to 74 years. The most commonly affected age group was 7-9 years (Fig.1). The socioeconomic status was poor in 37 (84%) patients. As shown in Table 1, trauma was found to be the most.common predisposing factor (57%). The most common site involved by infection was the tibia (27) followed by the femur (10) .

Among this group, thirty six cases (81%) showed
positive bacterial cultures, while in 8 cases (19%) no bacteria were isolated.
The cultures were pure in 30 (83%) cases while in 6 (17%) cases revealed
a mixed growth. Staphylococcus aureus was the most common causative
pathogen (45.2%) (Table 2). Two anaerobic organisms (Peptostreptococcus
anaerobius and Fusobacterium nucleatum) were isolated from one case with
acute osteomyelitis.
Exogenous osteomyelitis
The total number of cases were 62. The most
frequent predisposing factor was compound fracture (46). All cases
showed positive bacterial cultures. The cultures were pure in 50%
of cases. Pseudomonas species and Klebsiella species were the most
common isolates (17.5% each) followed by Proteus species (12.9%) Table
2.
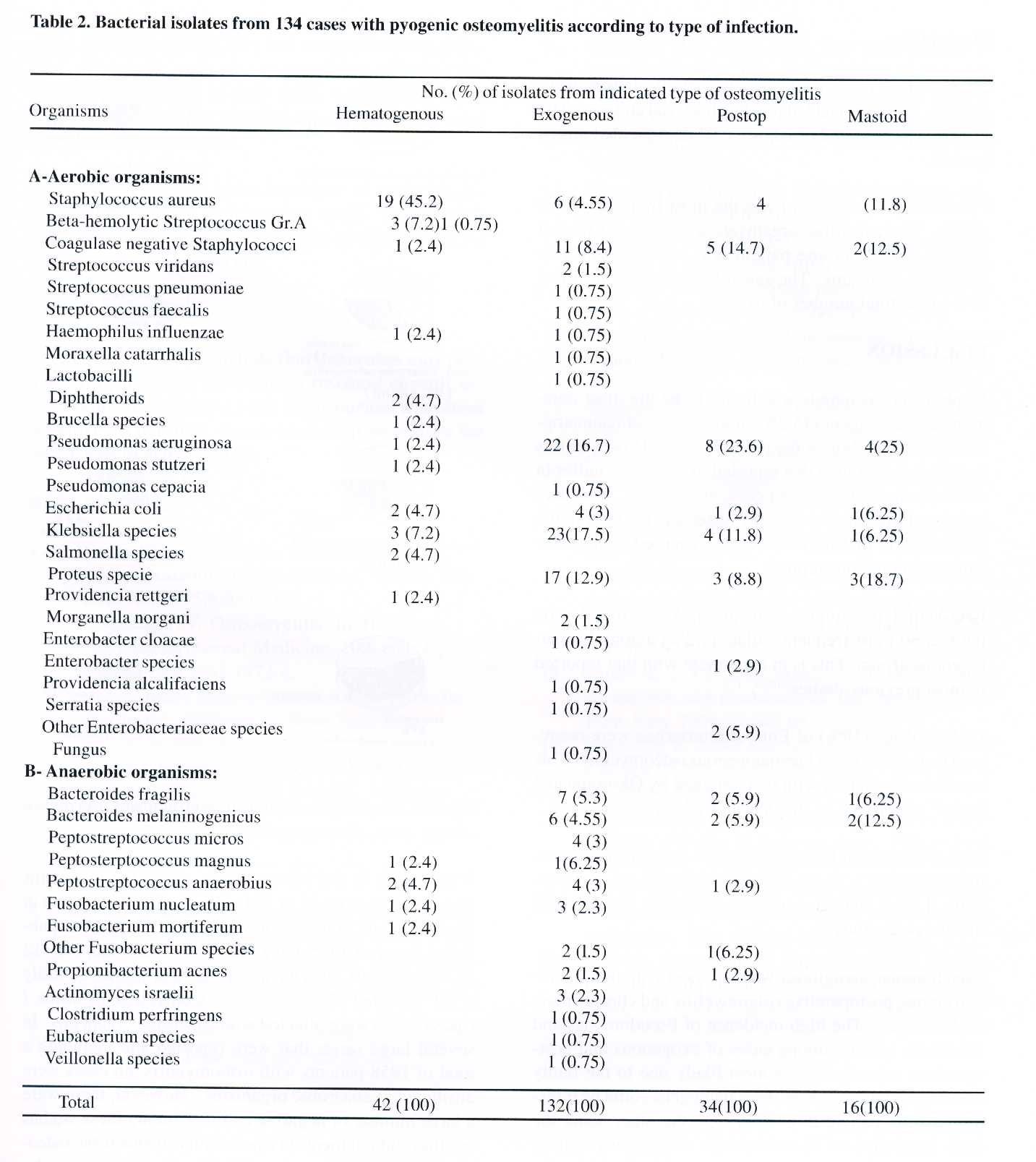
The anaerobic bacteria were isolated from 25 (40%) cases. All cases of anaerobic infection yielded mixed growth with aerobic bacteria except in one case. The anaerobic isolates constituted 34 out of 132 isolates (26%).
Postoperative osteomyelitis
The total number of cases was 21. The commonest operative procedure leading to osteomyelitis was extramedullary internal fixation (12), followed by hip replacement (4), intramedullary internal fixation (3), osteotomy (1) and application of bone cement (1) .
All cases included in this group yielded positive bacterial cultures. The isolated organisms were pure in 13 of cultures, while 8 of them revealed mixed growth as shown in Table 2.
The anaerobic organisms were isolated from 6 patients (28.6%). The anaerobic isolates constituted 18% of the total number of isolates. Five cases yielded anaerobes mixed with aerobic organisms, while one case yielded pure anaerobic isolate.
Mastoiditis
There were 7 cases in this group and all of them were chronic. All cases yielded positive bacterial cultures. The growth was pure in 2 of cultures, while 5 yielded mixed growth.
Pseudomonas aeruginosa was the most frequent isolate (25%). The anaerobic organisms were isolated from 4 patients (57%), as one patient was infected with two anaerobic organisms. The anaerobic isolates constituted 31% of the total number of isolates.
DISCUSSION
Staphylococcus aureus was found to be the most common causative agent (45.2%) among cases of haematogenous osteomyelitis in the present study. However, this incidence is less than that reported in previous studies in which the incidence was 61-96% of cases1,6-12. This may be related to isolation of many anaerobic bacteria in the present study that may have been regarded as negative cultures in previous reports.
Beta-hemolytic Streptococcus group-A was found to be the second most frequent isolate (7.2%) among haematogenous group. This is in agreement with that reported in most previous studies9,10,13.
Eight isolates (19%) of Enterobacteriaceae were recovered from the cases of haematogenous osteomyelitis. This somewhat coincides with that obtained by Okoroma and Agbo11 who found an incidence of 22.5%.
Pseudomonas and Klebsiella species were the most common isolates (17.5%) in the cases of erogenous osteomyelitis. Lower incidence of these organisms was reported in a previous study14.
Pseudomonas aeruginosa was the most common pathogen among postoperative osteomyelitis and chronic mastoiditis cases. The high incidence of Pseudomonas and Klebsiella species among cases of exogenous and postoperative osteomyelitis is most likely due to the faulty dressing technique where these pathogens could be transmitted from patient to another. On the other hand, the high incidence of Pseudomonas aeruginosa among chronic mastoiditis cases may be attributed to the misuse of antibiotic ear drops. The ear drops could transmit these bacteria from skin of the external ear into the middle ear through a perforated tympanic membrane and then these bacteria can settle into the mastoid bone.
Coagulase negative Staphylococci were found to be the second most common isolate (14.7%) among cases of postoperative bone infection. Stevens15 reported a slightly lower incidence (11%) of the same organisms.
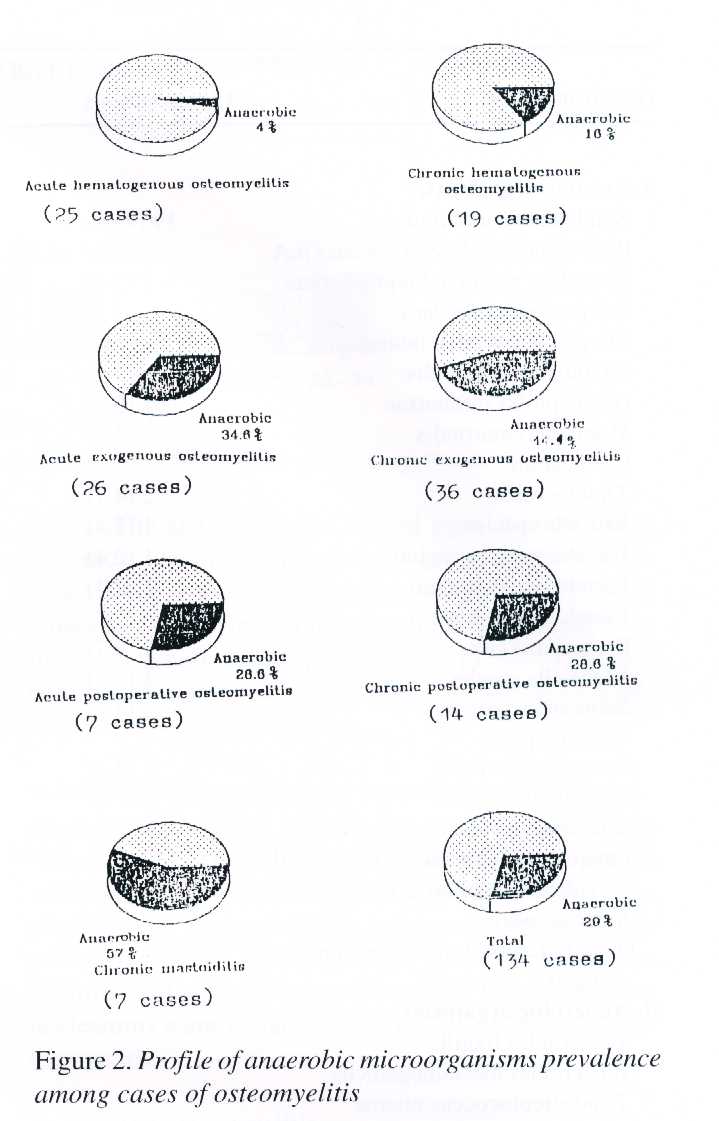
With regard to the present study, anaerobic organisms were isolated from 39 of 134 patients (29%) as shown in Fig 2. Raff and Melo16 reviewed large series of cases published between 1936 and 1976. They found that only 12 of 1603 cases (0.74%) has anaerobic bone infection. Kelly et al17 reported 257 cases with osteomyelitis, of which 7 cases (2.7%) were infected with anaerobic organisms. In several large series that were reported and including a total of 1958 patients with osteomyelitis, no cases were attributed to anaerobic organisms. However, there were a large number of negative cultures among these studies but they did not mention a possibility of anaerobic osteomyelitis among these cases1,6-12,18-21. The failure of isolation of anaerobes in the previous studies of bone infection might be related to disuse of optimal cultivation techniques for anaerobes and/or the anaerobic cultivation was not performed routinely for every case with osteomyelitis.
On the other hand, Lewis et al4 reported a higher incidence of anaerobic osteomyelitis than that obtained in the present study. They studied 58 cases with osteomyelitis, of which 23 (39.6%) had anaerobic bone infection. This high incidence of anaerobic osteomyelitis which was obtained in their study was thought to be due to the selection of resistant chronic cases that were referred to that hospital.
Hall et al22 reported a lower incidence of anaerobic osteomyelitis than that in the present study. They investigated 182 patients with osteomyelitis, of whom 40 (22%) had anaerobic bone infection.
CONCLUSION
From this study, we conclude that anaerobes may play a significant role in producing a resistant chronic osteomyelitis that does not yield to the normal treatment measures. Therefore, we advocate routine culture for anaerobes in osteomyelitis.
REFERENCES
1. Morrey BF, Peterson HA. Haematogenous
pyogenic osteomyelitis in children. Orthop Clin
North Am 1975;6:935-51.
2. Hirschmann JV. Osteomyelitis.
In: Harrison's Principles of Internal Medicine. 10th edn.
Japan: Mcgraw-Hill 1983:1972-4.
3. Nade S. Acute haematogenous osteomyelitis
in infancy and childhood. J Bone Joint Surg
1983;65-B:109-19.
4. Lewis RP, Sutter VL, Finegold SM. Bone
infections involving anaerobic bacteria. Medicine 1978;57:279-305.
5. Nakata MM, Lewis RP. Anaerobic bacteria
in bone and joint infections. Rev Infect Dis
1984;6:165-70.
6. Green M, Nyhan WL, Fousek MD. Acute
haematogenous osteomyelitis. Pediatrics 1956;17:368.
7. Dich VQ, Nelson JD, Haltalin
KC. Osteomyelitis in infants and children: a review of 163
cases. Am
J Dis Child 1975;129:1273-8.
8. Mollan RAB, Piggot J. Acute
osteomyelitis in children. J Bone Joint Surg 1977;59-B:2-7.
9. Gillespie WJ, Mayo KM. The management
of acute haematogenous osteomyelitis in the
antibiotic era.
J Bone Joint Surg l981;63-B:126-31.
10. Cole WG, Dalziel RE, Leitl S. Treatment of
acute osteomyelitis in childhood. J Bone Joint
Surg 1982;64-B:218-23.
11. Okoroma EO, Agbo DC. Childhood osteomyelitis.
Clin Pediatr 1984;63-B:548-52.
12. Lauschke FHM, Frey CT. Haematogenous
osteomyelitis in infants and children in
Northwestern Region
of Namibia: management and two-year results. J Bone Joint Surg
1994;76-A:502-10.
13. Caron HN, Behrendt H. Osteomyelitis in newborn
infants. Ned Tijdschr Geneeskd
1989;133:1651-4.
14. Gerszten E, Allison MJ, Dalton HP.
An epidemiologic study of 100 consecutive cases of
osteomyelitis.
South Med J 1970;63:365-7.
15. Stevens DB. Postoperative orthopaedic
infections. J Bone Joint Surg 1964;46-A:96.
16. Raff MJ, Melo JC. Anaerobic osteomyelitis.
Medicine 1978;57:83-103.
17. Kelly PJ, Wilkowske CJ, Washington JA,II.
Comparison of Gram-negative bacillary and
staphylococcal
osteomyelitis of the femur and tibia. Clin Orthop 1973;96:70-5.
18. Kulowski J. Pyogenic osteomyelitis of the
spine: an analysis and discussion of 102 cases. J
Bone Joint Surg
1936;16:343-64.
19. Shandling B. Acute haematogenous osteomyelitis:
a review of 300 cases treated during
1952-1959.
S Afr Med J 1960;34:520-4.
20. Winters JL, Cahen I. Acute haematogenous
osteomyelitis: a review of sixty-six cases. J
Bone Joint
Surg 1960;42-A:691-704.
21. Trunzo RG, Dowling JJ. Acute haematogenous
osteomyelitis of children in the era of broad spectrum antibiotics.
Clin Orthop 1962;22:108-25.
22. Hall BB, Rosenblatt JE, Fitzgerald
RH, Jr. Anaerobic septic arthritis and osteomyelitis.
Orthop Clin North
Am 1984;15:505-16.
----------------------------------------------------------------------------------
* Lecturer
Basrah University
Teaching Hospital
** Professor
Department of
Surgery
***Assistant Professor
Department of
Microbiology
College of Medicine
University
of Basrah
Iraq.

