Abdulaziz Al Mulhim, LM, JB, CAB (O& G)*
Objective: To determine
the incidence, epidemiology and antenatal complications of twin
gestation.
Setting: Department
of Obstetrics and Gynecology, King Fahad University hospital, Al-
Khobar, Saudi Arabia.
Subject and Design:
Two-hundred and twenty-seven (227) patients with twin gestation
that delivered over
an 8 year period were studied. The control group comprised of two
singleton deliveries
that followed immediately after the twins. Patients were divided
into
three groups according
to gestational age of the first, prenatal care and the total number
of antenatal visits
to the hospital.
Main outcome and result: The incidence of twin deliveries after 24 weeks gestation was ten per thousand. The majority of cases occurred in patients aged 20-30 years of parity 4 and above. There was a higher incidence of iron deficiency, anemia, pre-term labor, intrauterine growth retardation, pregnancy induced hypertension and intrauterine fetal death in the study group compared to the control.
Conclusion: Frequent prenatal visits, earlier diagnosis and management of several maternal complications would lower the incidence of perinatal morbidity and mortality. Early determination of zygosity is useful in establishing the prognostic categories of twin gestation. Further studies are needed to address the specific aspect of twin gestation in order to outline those areas for improvement of care in this challenging area of obstetrics.
Bahrain Med Bull 2001;23(2):56-60.
Twin gestations constitute less than 1% of all
births, yet they are responsible for a disproportionate amount of the overall
perinatal morbidity and mortality1. Several studies have suggested
that twin gestations impose greater demands on the maternal physiologic
systems than do singleton pregnancies2-4. It is generally believed
that an increased incidence of maternal complications in pregnancy is due
to this burden on the adaptive capacity of the mothers. Although
there is a large body of contemporary literature dealing with twin gestations,
only a few reports have specifically focused on the incidence of maternal
complications as they occur in twin gestations. Similarly, few reports
have examined other factors, such as maternal age, zygosity or variation
in prenatal care that might be related to the scope and magnitude of these
maternal complications.
The purpose of this study was to determine the incidence, epidemiology and antenatal complications of twin gestations seen at the King Fahad Hospital of the University, Al Khobar, Eastern Province, Saudi Arabia between January 1991 and December 1998.
METHODS
The case records of 227 patients with twin gestation that delivered during the period of study were reviewed. The control group comprised of two singleton deliveries that occurred immediately after a twin delivery giving a total of 454 patients.
Demographic data, past obstetric history of twins, mode of occurrence of the current pregnancy and antenatal complications during the index pregnancy were noted for the patients and control groups. In all cases, the diagnosis of twin gestations was based on clinical and ultrasound examinations. The patients with twins were divided into three groups based on the gestational age at the first prenatal care visit and the total number of visits as follows: Group 1 patients had prenatal care beginning before 24 weeks and had six or more prenatal clinic visits; Group 2 patients had prenatal care beginning after 24 weeks and had fewer than six prenatal clinic visits; Group 3 patients had no prenatal care during the pregnancy.
Facilities for cytogenetic and postmortem examinations were not available at the hospital. Statistical analysis was performed by means of the X2[AaM1] test with Bonferrori correction for multiple comparisons and values of P<0.005 were considered as significant by this method5.
RESULTS
The incidence of twin gestations of 24 or more
weeks that delivered during the 8 year study period is shown in table 1.
The incidence of twin gestation increased from 8/1000 in 1991 to 12/1000
in 1998 with an overall incidence of 10/1000 of all deliveries. Zygosity
was successfully determined by placental pathology or fetal sex in 87%
(197 patients). The overall
incidence of dizygotic twins in this series was
66% (150 patients), monozygotic was 21% (47 patients) and 13% (30
patients) was undetermined.


A maternal family history for twin pregnancy among first or second degree relatives was present in 10% (23 patients) 8.3% (19) of these were from patients with dizygotic pregnancies. None of the patients had a previous twin pregnancy. Spontaneous twinning occurred in 38% (87 patients), invitro fertilization and embryo transfer resulted in 12% (27 cases) and fertility drugs were used in 50% (113 cases) of twin gestations. The age distribution of the patients ranged from 16-44 years with a median of 29 years (Table 2). Primigravidas represented 20% (45 patients) of the group with an age range of 16-41 years (mean age was 22 years). Multigravida patients ranged between 17 and 43 years (mean age was 27 years) (Table 3). Group 1 constituted 4.6% (104 patients) of our study group, Group 2 patients 25% (57 patients) and Group 3, 29% (66 patients).

Table 4 shows the incidence of common complications
during pregnancy. The overall incidence of complications was 91%
(206) in the study. This was significantly higher compared with the
control group (33%). There was only a single antenatal complication
in 75% and multiple complications in 25% of the patients with twin pregnancy.
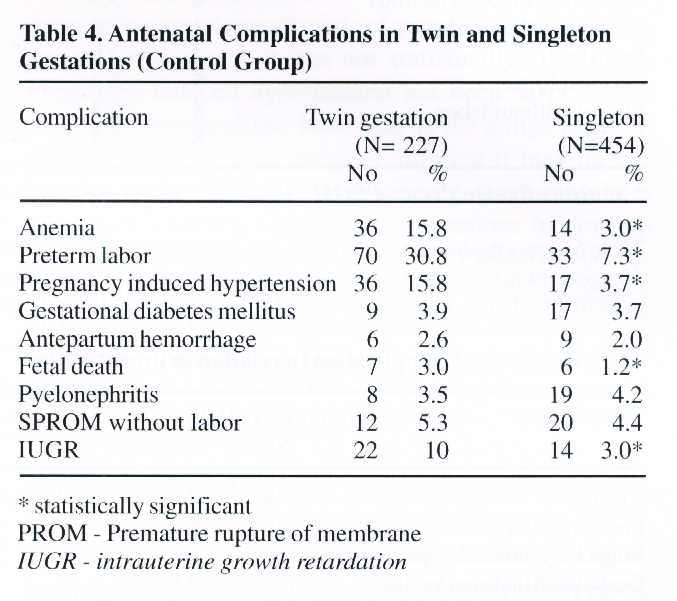
The most common complication, preterm labor (spontaneous onset of regular uterine contractions with progressive dilatation of the cervix before 37 weeks gestation) was nearly fourfold in twin gestations as compared with the singleton gestations (30.8% and 7.1% respectively). The incidence of induced hypertension (defined as a blood pressure of 140/90 mmHg or greater on two occasions 6 hours apart occurring after 20 weeks of gestation) was also significantly increased in twin gestation as compared with singleton ones (16.2% versus 3.7%). Intrauterine fetal death of one or both fetuses after 24 weeks gestational age occurred in 3% of twin gestation, a nearly threefold higher rate than in the singleton gestations (1.2%). Anemia [haemoglobin <10.0 g/dl] occurred in 16.2% of twin gestation, which was five times higher than in the control group (2.9%).
Intrauterine growth retardation [defined as fetal weight less than the tenth percentile for gestational age] occurred in 10% of twin gestation which was three times higher than singleton gestations (3%).
Other common complications like pyelonephritis (urine culture showing greater than 105 bacterial colonies per milliliter and maternal temperature of 380C with costovertebral angle tenderness), gestational diabetes mellitus (two or more elevated serum glucose levels in a 3 hour, 100g glucose tolerance test after overnight fasting), spontaneous premature rupture of membranes (confirmed by aseptic speculum examination) and antepartum hemorrhage (vaginal bleeding after 24 weeks gestation) were not significantly higher in twin gestations than in singletons.

Table 5 shows the incidence of pregnancy complications in relation to the zygosity. Pregnancy induced hypertension was more common in dizygotic twin pregnancies. However this frequency did not achieve significance when corrected by the Bonferrori method. Intrauterine growth retardation, intrauterine fetal death and preterm labor were more common among monozygotic twin gestations.
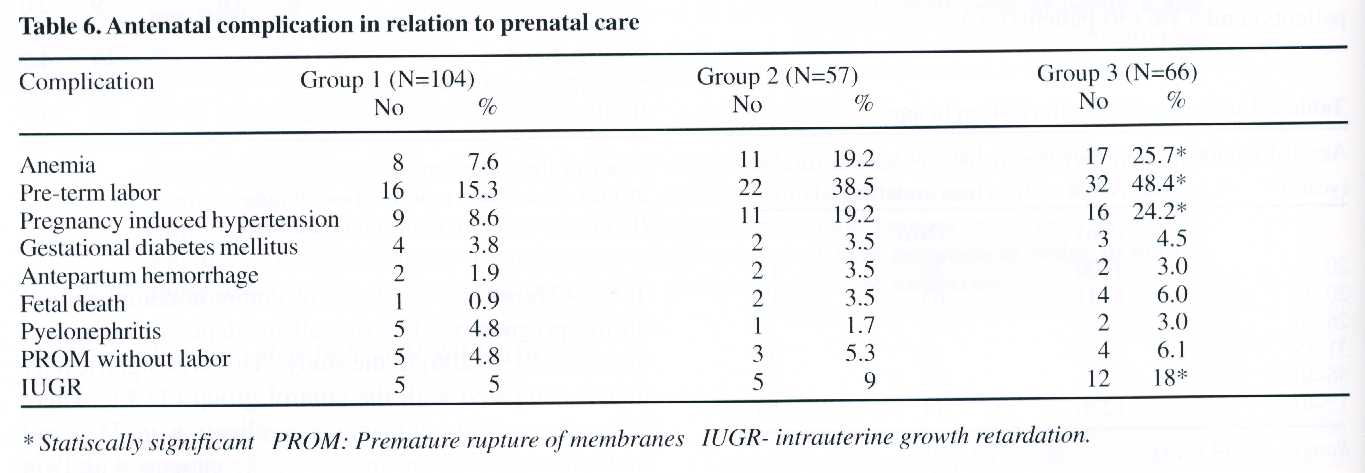
Table 6 shows the antenatal complications in the three groups of patients divided according to the prenatal care they received. Group 1 patients had the lowest incidence of complications. Group 2 patients had more complications than Group 1 except for pyelonephritis which was more frequent in Group 1. Group 3 patients had a significantly higher incidence of anemia, preterm labor, pregnancy induced hypertension, intrauterine fetal death and intrauterine growth retardation compared with group 1 patients.
DISCUSSION
The incidence of twinning varies widely throughout the world; the highest being reported in black populations, with Nigeria having a rate of 1 in 20 to 25 pregnancies2,3 and the lowest in Oriental populations4. In our study, there were 22,756 singleton gestations and 227 twin gestations during the study period giving an incidence of 1 in 100 pregnancies. The rate increased from 1991 to 1998 and this may be due to the increasing use of medications for ovulation induction and assisted methods for conception in the management of infertility. There were 140 (62%) twin gestations that resulted from ovulation induction and 27 of these from in-vitro fertilization and embryo transfer in the study. The remaining 87 (28%) cases were the result of spontaneous ovulation.
The rate of monozygotic twinning is fairly constant throughout the world at 3 to 5 per thousand deliveries2 but in our study, the incidence was slightly lower (2 per thousand).
Monozygotic twinning is thought to be due to chance, unrelated to heredity resulting from a delay in implantation associated with nutritional, hypoxic or other stress2. The incidence of dizygotic twinning ranges widely between 4 and 40 per 1,000 deliveries2, with 6 per 1000 deliveries in our study. The zygosity could not be determined in 30 (13%) cases of twins in the series which can be studied using enzymatic markers or dermatoglyphics.
Cameron determined 8% out of 45 % of twins with undiagnosed zygosity using these markers6. The incidence of twinning is affected by a variety of maternal characteristics that include age, parity, genetic predisposition and the use of fertility drugs6.
The mean maternal age in the twins was 31 years as compared with 25 years for singletons. Most studies have found that the incidence of twinning increases with advancing maternal age up till 35 years after which the rates decline2.
Maternal age is the only factor that may possibly affect rates of monozygotic twinning2. Heuser et al found the incidence of monozygotic twins to be 3 per 1,000 in women less than 20 years of age, while among women over 40 it was 4.5 per 1, 0007. This difference in the incidence is not as dramatic as that seen for dizygotic twinning, which increased from 2.5 per 1,000 in women 15-19 years of age to 11.5 per 1,000 in women 30-34 years of age8.
The twinning rate for primigravidas was 6 per 1,000 and 11 per 1,000 for multigravidas (P< 0.0001) in our study. Ghai and Vidyasagar found a rate of 21.3 per 1,000 among primigravidas as compared to 26 per 1,000 among multigravidas9.
The finding that twinning is more likely to occur among the higher parity patients has been shown to be independent of maternal age7. The issue of whether parity or gravidity is more influential in dizygotic twinning has not been fully examined. This may be true but, in our study about 140 sets of twins were due to the use of fertility drugs and assisted methods of conception.
Maternal family history for twin gestation among the first or second degree relatives was obtained in 23 (10%) patients, 19 (83%) of them were from patients with dizygotic gestations. There is no evidence that the incidence of monozygotic twinning increases with a family history of twins, but increased dizygotic twinning rates do seem to be affected by maternal familial influences as shown in our study. Mothers of dizygotic twins have been found more likely to have recurrent twin gestation than women who never had a twin gestation before6. White and Wyshak found that 17% of women who were twins themselves gave birth to twins, as compared to 0.8% of women whose husbands were twins10. These rates, when compared to the general population twinning rate of 1.1% illustrate that familial tendencies seem to be restricted to the maternal side.
Pre-term labor was overwhelmingly the most frequent complication in the series. Our incidence frequencies conform with those of other series11. We did not find a statistically significant correlation of preterm labor and zygosity.
The level of prenatal care has its benefits in patients with twin pregnancy as shown in our study, with lower rates of complications in patients with more frequent visits and early antenatal diagnosis. Some reports have suggested that bed rest and/or hospitalization increases the duration of gestation12. As a policy, strict bed rest and prophylactic tocolytic therapy was neither enforced nor quantitated in our study, we cannot support or refute this contention. Our incidence of pregnancy induced hypertension in the series (16%) compares favorably with 15-40% reported in the literature13. We also found that dizygotic twins are at greater risk of pregnancy induced hypertension although it was not statistically significant. Pregnancy induced hypertension has been suspected of having an immunologic basis and as the antigenecity of each fetus in dizygotic twins is different it may have a bearing to this finding14. Alternatively, there may be a hereditary tendency for dizygotic gestations to develop pregnancy induced hypertension15,16. Patients who received inadequate prenatal care had a higher incidence of pregnancy induced hypertension and also increased severity of the disease. The most likely explanation for this may be that the mild form of the condition remained undetected in these patients.
Intrauterine fetal death and intrauterine growth retardation were found to be more frequent in twin than in singleton pregnancy as reported by other authors17,18. Unfortunately, autopsies were not performed in any of our cases, so that etiologies could not be analyzed. We found that zygosity was significantly related to the incidence of fetal death and intrauterine growth retardation with monozygotic gestations suffering greater losses19,20. Other studies have also correlated placental membrane type to fetal death"-'g. Monochorionic placentas are always monozygotic and such placentas usually have fetal vascular anastomosis, although frank twin -twin transfusion is rare. However, mechanisms other than Twin-Twin transfusion syndrome but, related to vascular communication, have been found to be associated with fetal death and intrauterine growth retardation in twins21. We also found that levels of prenatal care were related significantly and inversely to fetal death rate and intrauterine growth retardation. Fetal malformation was not studied in the series due to non- availability of autopsy. Other complications such as antepartum haemorrhage, gestational diabetes mellitus, spontaneous rupture of membranes and pyelonephritis were not significantly higher in twin gestations than singleton ones in the series.
CONCLUSION
Prenatal care and early diagnosis is clearly advantageous to the patients as all the complications were increased in Group 2, highest in Group 3, least in Group 1, and hence would have a great impact on reducing the occurrence and severity of certain complications. Frequent prenatal visits, earlier diagnosis and management of several maternal complications would lower the incidences of perinatal morbidity and mortality in the patient group. In addition, it seems that early determination of zygosity is useful in establishing the prognostic categories of twin gestation. Further studies are needed to address the specific aspect of twin gestation in order to outline those areas for improvement of care in this challenging area of Obstetrics.
REFERENCES
1. Medearis AL, Jonas HS, Stockbaver JU, et al.
Perinatal death in Twin pregnancy. A five
year analysis
of statewide statistics in Missouri. Am J Obstet Gynecol 1979;134:413-21.
2. MacGillirray 1. Epidemiology of
twin pregnancy. Semin Perinatal 1986;10:4-8
3. MacGillirray 1. Twin and other
multiple deliveries. Clin Obstet Gynecol 1980;7:581-600.
4. Marivate M, Norman RJ.
Twins. Clin Obstet Gynecol 1982;9:723-43.
5. Wimer BJ. Statistical Principles
in Experimental Design. USA:McGraw Hills, 1962:85-92.
6. Cameron AHD. The Birmingham
Twin Survey. Pro Royal Society Med 1968;61:229-34.
7. Heuser RL. Multiple births.
United States - 1964. Washington DC: National Center for
Health Statistics,
1967. [DHEW (Series 21, No.14)].
8. Benirschke K. Multiple gestation: Incidence,
etiology and inheritance. In: Creasy R, Resnik
R, eds.
Maternal Fetal Medicine Principles and Practices. Philadelphia:WB
Saunders,
1989:565.
9. Ghai V, Vidyasagar D. Morbidity and
mortality factors in twins: An epidemiologic
Approach. Clin Perinatal 1988;15:565.
10. White C, Wyshak G. Inheritance
of human dizygotic twinning. New Engl J Med
1964;27:1003
11. De Muylder X, Moutquin YM, Desgranges
MF, et al. Obstetrical profile of twin
pregnancy.
Acta Genet Med Gemeliol (Roma) 1982;31:149-158.
12. Hawrylyshyn PA, Barkin M, Bernstein
A, et al. Twin pregnancies. A continuing
perinatal challenge. Obstet Gynecol
1982;59: 463-66.
13. Mc Mullen PF, Norman RJ,
Marivate M. Pregnancy induced hypertension in twin
pregnancy.
Br J Obstet Gynaecol 1984;91:240-43.
14. Benirschke K, Kim CK. Multiple
pregancy. N Engl J Med 1973;288:1278-84.
15. Chesley IC, Cooper DW.
Genetics of hypertension in pregnancy with a possible single
gene control
of preeclampsia and eclampsia in descendants of eclamptic women.
Br J
Obstet Gynecol
1986;93:898-908.
16. Coonrad DV, Hickok DE, Zhu K,
et al. Risk factors for preeclampsia in twin pregnancies.
A population
based cohort study. Obstet Gynecol 1995;85:645.
17. Devoe LD, Azor H. Simultaneous
non stress fetal heart rate history in twin pregnancy.
Obstet Gynecol
1981;58:450-55.
18. Manning FA. Fetal biophysical
profile scoring in Fetal Medicine: Principles and practice.
Norwalk
CT: Appleton and lange, 1995:288.
19. Benivschke K. Twin placenta in perinatal
mortality. NY state J Med 1961;61:1499-507.
20. Bayoria R, Wiggles worth J, Fisk NM.
Angio architecture of monocharionic placentas in
relation
to the twin-twin transfusion syndrome. AM J Obstet Gynecol 1995;172:856.
21. Kuala A, Louppila P, Koivisto
M, et al. Twin pregnancy: A clinical study of 335 cases.
Acta Obstet
Gynecol Scand (suppl) 1975;44:5-12.
-----------------------------------------------------------------------------------------------
* Associate Professor and Consultant
Department of Obstetrics &Gynecology
College of Medicine, King
Faisal University
Dammam, Saudia Arabia

