BLOOD
DISEASES
William harvey 1578 – 1657
Is an English doctor, who discovered
the circulation of the blood and the role of the heart in propelling it, thus
refuting the theories of Galen and laying the foundation for modern physiology.
Born on  five years under the celebrated
anatomist Fabricius, who was already studying the
valves of the veins. Having earned a medical degree
five years under the celebrated
anatomist Fabricius, who was already studying the
valves of the veins. Having earned a medical degree

From 1615 to 1656

Karl Landsteiner 1868 – 1943
 Born in
Born in
Blood Type
is classification of red blood cells by the presence of specific substances on
their surface. Typing of red blood cells is a prerequisite for blood
transfusion. In the early part of the 20th century doctors
discovered that blood transfusions often failed because the blood type of the
recipient was not compatible with that of the donor. In 1901 the Austrian
pathologist Karl Landsteiner
classified blood types and discovered that they were transmitted by Mendelian heredity according to Mendel's Laws.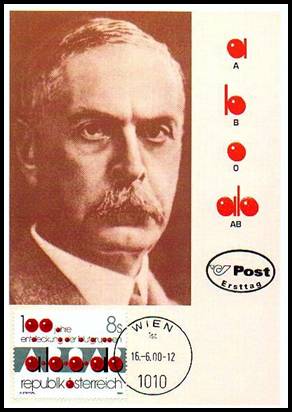
The four blood types are known as A, B, AB, and O. Blood type A contains red blood cells that have a substance A on
their surface. This type of blood also contains an antibody directed against
substance B, found on the red cells of individuals with blood type B. Type B
blood contains the reverse combination. Serum of blood type AB contains neither
antibody, but red cells in this type of blood contain both A and B substances.
In type O blood, neither substance is present on the red cells, but the
individual is capable of forming antibodies directed against red cells
containing substance A or B. If blood type A is transfused into a person with B
type blood, anti-A antibodies in the recipient will
destroy the transfused A red cells. Because O type blood has neither substance
on its red cells, it can be given successfully to almost any  person. Individuals with blood type
AB have no antibodies and can receive any of the four types of blood; thus
blood types O and AB are called universal donors and universal recipients,
respectively.
person. Individuals with blood type
AB have no antibodies and can receive any of the four types of blood; thus
blood types O and AB are called universal donors and universal recipients,
respectively.
Other hereditary blood-group systems
have subsequently been discovered. The hereditary blood constituent called Rh factor is of
great importance in obstetrics and blood transfusions because it creates
reactions that can threaten the life of newborn infants. Blood types M and N have importance in legal cases involving proof of paternity.
Disorders of the blood arise from
abnormal changes in its composition. An abnormal reduction in the  hemoglobin content or in the number
of red blood cells is known as anemia,
which is regarded as a symptom rather than a disease and has a number of
causes. Probably the most common cause is blood loss or hemorrhage. Excessive
destruction of the red blood cells a condition known as hemolytic anemia may be
caused by a variety of toxins or by an antibody to the red blood cells. One
type that occurs in the infant at or shortly before birth is erythroblastosis fetalis.
hemoglobin content or in the number
of red blood cells is known as anemia,
which is regarded as a symptom rather than a disease and has a number of
causes. Probably the most common cause is blood loss or hemorrhage. Excessive
destruction of the red blood cells a condition known as hemolytic anemia may be
caused by a variety of toxins or by an antibody to the red blood cells. One
type that occurs in the infant at or shortly before birth is erythroblastosis fetalis.
 Anemia also results from decreased
production of red cells, attributable to a loss of iron, to a deficiency of
vitamin B12 or to a failure in the function of bone marrow. Finally one group
of anemias is caused by inherited defects in the
production of red cells (hemoglobin). These anemias
include a number of hereditary disorders in which the red cells lack any one of
several enzymes needed if the cell is to utilize glucose effectively.
Anemia also results from decreased
production of red cells, attributable to a loss of iron, to a deficiency of
vitamin B12 or to a failure in the function of bone marrow. Finally one group
of anemias is caused by inherited defects in the
production of red cells (hemoglobin). These anemias
include a number of hereditary disorders in which the red cells lack any one of
several enzymes needed if the cell is to utilize glucose effectively.
Formation of abnormal hemoglobin is
responsible for the hereditary defects called sickle-cell anemia and thalassemia
major. Both are severe diseases that can be fatal in childhood.
An increase in the number of
circulating red blood cells is called polycythemia, which can be a primary condition or one that follows
decreased oxygenation of the blood or hypoxia.
Extreme hypoxia occurs most commonly in advanced lung disease in certain types
of congenital heart disease and at high altitudes.
Leukemia is
accompanied by a disordered proliferation of white blood cells. Several types
of leukemia exist each characterized by the cells  involved.
involved.

A deficiency in any of the factors
necessary for blood coagulation leads to excessive bleeding. A decrease in
platelets is known as thrombocytopenia;
a decrease in clotting factor VIII results in hemophilia A; a decrease in clotting factor IX results in hemophilia B commonly known as Christmas disease. Several of the
hemorrhagic diseases such as hemophilia are hereditary. Preparations are
available that contain some of the clotting factors in concentrated form for
treating some of these disorders. In 1984 researchers developed a genetic
engineering technique for making factor VIII a blood-clotting factor of vital
importance for victims of the most common form of hemophilia.
Although clot formation is a normal
process it sometimes occurs inappropriately and constitutes a threat to life.
In patients hospitalized for a long time for example clots sometimes form in
the large veins of the legs. If these clots or thrombi travel to the lungs they
can cause death as a result of an embolism. Such venous thrombi are dissolved
in many cases with a combination of drugs that prevent coagulation and break
down clots. Anticoagulants include the natural compound heparin prepared from
the lungs and livers of animals and the synthetic chemicals dicumarol
and warfarin. Clot-dissolving drugs called thrombolytics include two enzymes urokinase
and streptokinase approved for medical use in 1979 and tissue plasminogen activator (TPA) a product of genetic
engineering.
Interaction of thrombocytes
with the fatty deposits found in atherosclerotic heart disease is thought to
contribute to heart attacks. Compounds such as aspirin and sulphinpyrazone,
which inhibit platelet activity, may decrease heart attacks in persons with
atherosclerotic disease.
![]()