|

Doctors
General Public
Medical
Students
Main
Page


| |
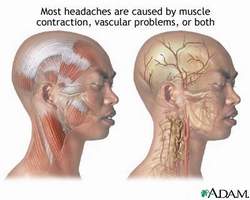
Complete Information on Headaches
 

Common causes of Headaches
| Chronic fatigue |
Emotional Stress |
Hormonal fluctuations |
| Weather/Seasonal
changes |
Travel through time
zones |
Altitudes |
| Skipping/delaying meals |
Sensory stimuli |
Medications |
| Caffeine |
Certain foods |
Alcohol |
Types of Headache
Urgent Headaches
Urgent headaches may be immediately life-threatening, and should be treated promptly.
Subarachnoid hemorrhage ("aneurysm")
Patients typically describe a headache related to a leaking aneurysm as a sudden, "thunderclap" headache, often the "worst
headache of my life" (an "aneurysm" is a swelling of a blood vessel in the brain). After this sudden onset, the pain may persist at
a high or low intensity for days. Abnormal neurological symptoms may occur, including brief loss of consciousness at the onset
of the headache, a stiff neck, or eye movement abnormalities.
Such a headache mandates prompt evaluation by a physician, since a missed aneurysmal leak can result in a catastrophic stroke
or death. Evaluation typically takes place in an emergency department, and includes a brain computed tomography (CT) scan.
A spinal tap (looking for leaked red blood cells) may be necessary to completely rule out the diagnosis. An MRI may be useful,
but typically requires neurology or neurosurgery consultation.
The definitive treatment for subarachnoid bleeding is surgery, although calcium channel blocking drugs (tioclodipine) may limit
damage.
Temporal (giant cell) arteritis
Patients with temporal arteritis (TA, an inflammatory process involving the walls of medium-sized arteries) are usually over age
50. Its symptoms are newly experienced localized headache, scalp tenderness and diminished pulse over the temple area ,
fevers, and aches. An unusual symptom highly suggestive of TA is "jaw claudication," or cramping of the jaws while chewing.
Blindness (due to involvement of the ophthalmic artery) is a frequent complication, and may be prevented with prompt therapy.
Blood tests reveal intense inflammation (with a high "ESR" test), and definitive diagnosis is made by finding inflammation on a
biopsy specimen taken from the temporal artery.
Treatment consists of prompt therapy with high-dose corticosteroids (such as prednisone), which should be instituted if the
syndrome is suspected (even before definitive biopsy results return.
Bacterial meningitis
Acute bacterial meningitis is a virulent infection, and is typically manifest by an ill-appearance, fever, headache, stiff neck, and
photophobia (avoidance of bright light). A rash may be present some forms.
Diagnosis consists of a spinal tap showing white blood cells, chemical tests, and bacteriology studies.
Treatment requires prompt antibiotic therapy.
CT scans and MRIs
While a "negative" CT of the brain is reassuring, the cost of imaging every person with headache is prohibitive (up to $3
billion/year in the US). Moreover, a CT scan will find a identifiable cause of headache (blood, tumor) in no more than 0.5 to
2.5% of patients, and most of these patients have abnormal clinical findings.
Indications for immediate CT Scan or MRI for Headache
| " Worst headache
of my life " |
| Headache onset after
exertion |
| Decreased alertness |
| Stiff neck |
| Abnormal neurological
findings |
| Decline during
observation |
| New headache lasting
> 2 months in patient 40-60 years old |

Special Headaches
Brain tumor
Though a fear for many headache sufferers, brain tumors are uncommon. Indeed, fewer than 20% of patients with brain tumors
experience only headache as a symptom (the most frequent symptom is seizure and/or neurological abnormality on exam).
Waking with a headache is said to be an important sign of a tumor-related headache, although this occurs frequently in chronic
headaches
Diagnosis is based on brain imaging and biopsy.
Treatment is determined by an oncologist in consultation with a neurosurgeon.
Cluster Headache
Cluster headache commonly affects young- to middle-aged men. It is of short duration (30-90 minutes) and causes headache
behind one eye, with eye redness, tearing, and nasal stuffiness on the involved side. Headaches are clustered over time (often
separated by weeks to months); in times of headache activity, headaches may occur up to 6 times a day, often causing
insomnia.
Diagnosis is based on its classic presentation.
Treatment includes high-dose anti-inflammatory medications (ibuprofen, others). For unknown reasons, over half get relief from
breathing 100% oxygen by face mask.
Coital Headache
Coital headache occurs around the time of intercourse, and lasts from minutes to hours, and may be indistinguishable from
subarachnoid hemorrhage.
Diagnosis may require CT and spinal tap to rule out subarachnoid hemorrhage.
Sinus Headache
Typically occurring in conjunction with upper respiratory tract infection or allergic rhinitis/sinusitis, sinus headache is usually dull
and constant, worse when bending forward, and may be associated with colored nasal discharge.
Diagnosis may be made clinically, by x-rays, or on CT.
Treatment is based on cause (antibiotics if bacterial, antihistamines/decongestants/intranasal steroids if allergic), and are
supplemented by interventions to promote drainage (brief course of nasal spray, intranasal saline mist).
Eye Strain Headache
This headaches is associated with prolonged reading or staring at a computer screen (but not with astigmatism or refractive
errors).
Hormonal Headache
While temporally related to menstrual cycle, menopausal flushing, or hormone use (oral contraceptives), this headache has no
distinguishing features otherwise.
Pain tends to diminish cyclically, or after menopause is completed (but only in 1/3 who develop menopausal headaches), or
after hormone discontinuation.
Benign Intracranial Hypertension
Also known as "pseudotumor cerebri," this syndrome typically affects young, overweight women on certain medications (oral
contraceptives, tetracycline, certain steroids, or vitamin A). The headache itself is nondescript, but exam findings include
swelling of the optic nerve, which usually raises the specter of brain tumor.
CT scan looks essentially normal, and a spinal tap reveals high pressure.
Therapy includes corticosteroids.
Post-Traumatic Headache (Concussion)
"Concussion" is defined as loss of consciousness associated with head injury. Symptoms include headache, dizziness, and
confusion; long-term symptoms are headache, irritability, fatigue, anxiety, insomnia, memory disturbance, and impaired
concentration may persist for up to 18 months.
A CT scan is typically normal.
Treatment involves support with mild analgesia and reassurance.
Migraine With Aura (Classic Migraine)
A typical headache is heralded by an aura (blinking lights with partial vision loss, then sight restoration) followed in 25 to 60
minutes by a throbbing, unilateral headache associated with nausea, vomiting, and photophobia lasting 6-8 hours.
Abortive treatment includes non-steroidal anti-inflammatory medications, anti-nausea medications, ergot derivatives, and other
agents; preventive treatment involves various agents (see article on Migraine).
Common Headaches
While these headaches may have somewhat different causes, their manifestations (and treatment) are similar. Both may be
triggered by stress.
Migraine Without Aura (Common Migraine)
Migraine headache tends to be throbbing and one-sided (typically over the temporal area), and precipitated by certain foods,
strong smells, or the menstrual cycle (the ratio of female to male sufferers is 3 to 1). The time of day of onset varies.
Diagnosis is based on symptoms and lack of neurological abnormalities.
Treatment is the same as above.
Tension Headache
Often located in a both-sided "hatband" and neck distribution, tension headache is constant, precipitated by stress, has no
associated symptoms, and usually occurs later in the day; female to male ratio is 1 to 1.
Diagnosis is by clinical characteristics.
Treatment involves a step-wise approach, beginning with over-the-counter non-steroidal medications or acetaminophen,
followed by prescription-strength doses when necessary. Worse headaches may require migraine-type medications, such as
Midrin (isometheptene, dichloralphenazone, and acetaminophen). Medications containing caffeine or butalbital are sometimes
used (though risk of rebound headache increases). Prophylactic treatments similar to those used for migraine may be useful.
Emed
|