Electrolyte and Metabolic Abnormalities
In addition to the structural and functional cardiac conditions already discussed, numerous systemic metabolic aberrations affect the ECG, including electrolyte abnormalities and acid-base disorders, as well as systemic hypothermia.
CALCIUM
Hypercalcemia and hypocalcemia predominantly alter the action potential duration. An increased extracellular calcium concentration shortens the ventricular action potential duration by shortening phase 2 of the action potential. In contrast, hypocalcemia prolongs phase 2 of the action potential. These cellular changes correlate with abbreviation and prolongation of the QT interval (ST segment portion) with hypercalcemia and hypocalcemia, respectively. Severe hypercalcemia (e.g., serum Ca2+ ³15 mg/dl) can also be associated with decreased T wave amplitude, sometimes with T wave notching or inversion. Hypercalcemia sometimes produces a high takeoff of the ST segment in leads V1 and V2 and can thus simulate acute ischemia.
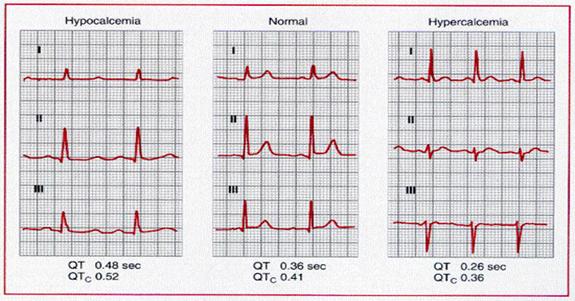
Prolongation of the QT
interval (ST segment portion) is typical of hypocalcemia. Hypercalcemia may
cause abbreviation of the ST segment and shortening of the QT interval.
 Hyperkalemia
is associated with a distinctive sequence of ECG changes. The earliest effect is
usually narrowing and peaking (tenting) of the T wave. The QT interval is
shortened at this stage associated with decreased action potential duration.
Progressive extracellular hyperkalemia reduces atrial and ventricular resting
membrane potentials, thereby inactivating sodium channels, which decreases Vmax
and conduction velocity. The QRS begins to widen and P wave amplitude decreases.
PR interval prolongation can occur, followed sometimes by second- or
third-degree AV block. Complete loss of P waves may be associated with a
junctional escape rhythm or sinoventricular rhythm. In the latter
instance, sinus rhythm persists with conduction between the SA and AV nodes and
occurs without producing an overt P wave. Moderate to severe hyperkalemia
occasionally induces ST elevations in the right precordial leads (V1
and V2) and simulates an ischemic current-of-injury pattern. However,
even severe hyperkalemia can be associated with atypical or nondiagnostic ECG
findings. Very marked hyperkalemia leads to eventual asystole, sometimes
preceded by a slow undulatory (sine-wave) ventricular flutter-like pattern. The
ECG triad of (1) peaked T waves (from hyperkalemia), (2) QT prolongation (from
hypocalcemia), and (3) LVH (from hypertension) is strongly suggestive of chronic
renal failure.
Hyperkalemia
is associated with a distinctive sequence of ECG changes. The earliest effect is
usually narrowing and peaking (tenting) of the T wave. The QT interval is
shortened at this stage associated with decreased action potential duration.
Progressive extracellular hyperkalemia reduces atrial and ventricular resting
membrane potentials, thereby inactivating sodium channels, which decreases Vmax
and conduction velocity. The QRS begins to widen and P wave amplitude decreases.
PR interval prolongation can occur, followed sometimes by second- or
third-degree AV block. Complete loss of P waves may be associated with a
junctional escape rhythm or sinoventricular rhythm. In the latter
instance, sinus rhythm persists with conduction between the SA and AV nodes and
occurs without producing an overt P wave. Moderate to severe hyperkalemia
occasionally induces ST elevations in the right precordial leads (V1
and V2) and simulates an ischemic current-of-injury pattern. However,
even severe hyperkalemia can be associated with atypical or nondiagnostic ECG
findings. Very marked hyperkalemia leads to eventual asystole, sometimes
preceded by a slow undulatory (sine-wave) ventricular flutter-like pattern. The
ECG triad of (1) peaked T waves (from hyperkalemia), (2) QT prolongation (from
hypocalcemia), and (3) LVH (from hypertension) is strongly suggestive of chronic
renal failure.
Electrocardiographic
changes in hyperkalemia (A) and hypokalemia (B). A, On day 1, at a K+
level of 8.6 mEq/liter, the P wave
is no longer recognizable and the QRS complex is diffusely prolonged. Initial
and terminal QRS delay is characteristic of K+
-induced intraventricular conduction
slowing and is best illustrated in leads V2
and V6.
On day 2, at a K+ level
of 5.8 mEq/liter, the P wave is recognizable with a PR interval of 0.24 seconds,
the duration of the QRS complex is approximately 0.10 seconds, and the T waves
are characteristically “tented.” B, On day 1, at a K+
level of 1.5 mEq/liter, the T and U
waves are merged. The U wave is prominent and the QU interval prolonged. On day
4, at a K+ level
of 3.7 mEq/liter, the tracing is normal.
The electrophysiological changes associated with hypokalemia, in contrast, include hyperpolarization of myocardial cell membranes and increased action potential duration. The major ECG manifestations are ST depression with flattened T waves and increased U wave prominence. The U waves can exceed the amplitude of T waves. Hypokalemia is an important cause of acquired long QT(U) syndrome that predisposes to torsades de pointes. Hypokalemia also predisposes to tachyarrhythmias from digitalis.
Specific ECG effects of mild to moderate isolated abnormalities in magnesium ion concentration are not well characterized. Severe hypermagnesemia can cause AV and intraventricular conduction disturbances that may culminate in complete heart block and cardiac arrest (Mg2+ >15 mEq/L). Hypomagnesemia is usually associated with hypocalcemia or hypokalemia. Hypomagnesemia can potentiate certain digitalis toxic arrhythmias.
Isolated hypernatremia or hyponatremia does not produce consistent effects on the ECG. Acidemia and alkalemia are often associated with hyperkalemia and hypokalemia, respectively. Systemic hypothermia may be associated with the appearance of a distinctive convex elevation at the junction (J point) of the ST segment and QRS complex (J wave or Osborn wave). The cellular mechanism of this type of pathological J wave appears to be related to an epicardial-endocardial voltage gradient associated with the localized appearance of a prominent epicardial action potential notch.

Systemic hypothermia. The
arrows (V3 through
V6 ) point to the
characteristic convex J waves, termed Osborn waves. Prominent sinus bradycardia
is also present.
Nonspecific QRS and ST-T Changes
Low QRS voltage is said to be
present when the total amplitude of the QRS complexes in each of the six
extremity leads is 0.5 mV or less or 1.0 mV or less in leads V1
through V6. Low QRS voltage can relate to a variety of mechanisms,
including increased insulation of the heart by air (chronic obstructive
pulmonary disease) or adipose tissue (obesity); replacement of myocardium, for
example, by fibrous tissue (ischemic or nonischemic cardiomyopathy), amyloid, or
tumor; or short-circuiting effects (pericardial or pleural effusions). The
combination of relatively low limb voltage (QRS voltage
![]() 0.8 mV in
each of the limb leads), relatively prominent QRS voltage in
the chest leads (SV1 or SV2+RV5 or RV6
³3.5 mV), and poor R wave progression
(R wave less than the S wave in V1 through V4) has been
reported as a relatively specific, but not sensitive sign of dilated-type
cardiomyopathies (ECG–congestive heart failure triad).
0.8 mV in
each of the limb leads), relatively prominent QRS voltage in
the chest leads (SV1 or SV2+RV5 or RV6
³3.5 mV), and poor R wave progression
(R wave less than the S wave in V1 through V4) has been
reported as a relatively specific, but not sensitive sign of dilated-type
cardiomyopathies (ECG–congestive heart failure triad).
Multiple factors in addition to ischemia (e.g., postural changes, meals, drugs, hypertrophy, electrolyte and metabolic disorders, central nervous system lesions, infections, pulmonary diseases) can affect the ECG.Ventricular repolarization is particularly sensitive to these effects, which can lead to a variety of nonspecific ST-T changes. The term is usually applied to slight ST depression or T wave inversion or to T wave flattening without evident cause. Care must be taken to not overinterpret such changes, especially in subjects with a low prior probability of heart disease. At the same time, subtle repolarization abnormalities can be markers of coronary or hypertensive heart disease or other types of structural heart disease and probably account for the association of relatively minor but persistent nonspecific ST-T changes with increased cardiovascular mortality in middle-aged men.
The
term alternans applies to conditions characterized by the sudden
appearance of a periodic beat-to-beat change in some aspect of cardiac
electrical or mechanical behavior. These abrupt changes (AAAA
![]() ABAB
pattern) are reminiscent of a generic class of subharmonic (period-doubling)
bifurcation patterns, well described in perturbed nonlinear control systems.
Many different examples of electrical alternans have been described clinically;
a number of others have been reported in the laboratory. Most familiar is total
electrical alternans with sinus tachycardia, a specific but not highly sensitive
marker of pericardial effusion with tamponade physiology. This finding is
associated with an abrupt transition from a 1:1 to a 2:1 pattern in the
“to-fro” swinging motion of the heart in the effusion. Other alternans
patterns are due to primary electrical rather than mechanical causes. ST-T
alternans has long been recognized as a marker of electrical instability in
acute ischemia, where it may precede ventricular tachyarrhythmia. Considerable
interest has recently been shown in the detection of microvolt T wave (or ST-T)
alternans as a noninvasive marker of the risk of ventricular tachyarrhythmia in
patients with chronic heart disease. Similarly, TU wave alternans
may be a
ABAB
pattern) are reminiscent of a generic class of subharmonic (period-doubling)
bifurcation patterns, well described in perturbed nonlinear control systems.
Many different examples of electrical alternans have been described clinically;
a number of others have been reported in the laboratory. Most familiar is total
electrical alternans with sinus tachycardia, a specific but not highly sensitive
marker of pericardial effusion with tamponade physiology. This finding is
associated with an abrupt transition from a 1:1 to a 2:1 pattern in the
“to-fro” swinging motion of the heart in the effusion. Other alternans
patterns are due to primary electrical rather than mechanical causes. ST-T
alternans has long been recognized as a marker of electrical instability in
acute ischemia, where it may precede ventricular tachyarrhythmia. Considerable
interest has recently been shown in the detection of microvolt T wave (or ST-T)
alternans as a noninvasive marker of the risk of ventricular tachyarrhythmia in
patients with chronic heart disease. Similarly, TU wave alternans
may be a
 marker
of imminent risk of a ventricular tachyarrhythmia such as torsades de pointes in
hereditary or acquired long QT syndromes.
marker
of imminent risk of a ventricular tachyarrhythmia such as torsades de pointes in
hereditary or acquired long QT syndromes.
Prinzmetal angina with ST
segment and T wave alternans. B, ST segment and T wave alternans associated with
nonsustained ventricular tachycardia

Total electrical alternans (P-QRS-T) caused by pericardial
effusion with tamponade. This finding, particularly in concert with sinus
tachycardia and relatively low voltage, is a highly specific, although not
sensitive marker of cardiac tamponade.
 The
QT(U) interval is prolonged and measures approximately 600 milliseconds with TU
wave alternans. The tracing was recorded in a patient with chronic renal disease
shortly following dialysis. This type of repolarization alternans may be a
precursor to torsades de pointes.
The
QT(U) interval is prolonged and measures approximately 600 milliseconds with TU
wave alternans. The tracing was recorded in a patient with chronic renal disease
shortly following dialysis. This type of repolarization alternans may be a
precursor to torsades de pointes.