

Methods of Measuring Obesity,
with Special Emphasis
on
Children and Adolescents
Anissa M. Al-Sindi, BSc, MSc*
Several methods were used to determine obesity. The aim of this paper was to highlight the main methods used to measure obesity, with special emphasis on children and adolescents. Anthropometric measurements are widely used and these include weight and height, relative weight, body mass index, skinfold thickness, waist and waist-hip circumference ratio. The visibility and accuracy of these methods were briefly discussed. The classification of obesity based on weight and height and body mass index (BMI) for children was highlighted. In this region and due to lack of facilities and trained people, simple methods such as BMI is recommended to be used, especially with the availability of international reference data for BMI.
Bahrain Med Bull 2000;22(3):
Obesity is now becoming a major clinical and public health concern contributing to increasing morbidity and mortality rates for several chronic diseases, and affecting both adult and child populations worldwide.
The specific causes of obesity are poorly understood, but a wide variety of environmental, socio-economic, familial as well as individual variables appear to influence its development. Obesity often occurs as a result of small shifts in the energy homeostasis, which over time lead to a gradual but sustained weight gain. The aim of this paper is to highlight the main methods used to measure obesity.
Adult vs. childhood obesity
In adults,
obesity and overweight are often determined using the body mass index (BMI).
Adults are classified as obese or overweight by a variety of cut-off values
based on the mortality and morbidity associated with various levels of
weight. It is well established that obesity is a risk factor for chronic
diseases such as heart disease, hypertension, stroke, diabetes and some
forms of cancer1. Recently the World Health Organisation has published
non-gender specific BMI criteria for overweight and obesity in adults.
A BMI value of 25-29.9 indicates overweight whereas a BMI value of 30 indicates
obesity. The category of obesity is further classified into class
I (BMI 30-34.9), class II (BMI 35-39.9) and class III (BMI 40)2.
The waist circumference and the waist hip circumference ratio, which are measures of intra-abdominal fat, are often used to predict the health consequences of obesity in adults, as changes in these measurements tend to reflect changes in risk factors for cardiovascular diseases and other chronic illnesses.
Obesity in children and adolescents is difficult to quantify and until recently there has been little agreement on a common definition and a system of classification of obesity in the paediatric group. This is largely because of the increase in weight for height, sexual maturation and the changing body composition that characterizes child growth. Various methods have been used to assess adiposity in children including absolute weight, weight for height percentiles, percent of ideal body weight, body mass index and skinfold.
Measurements of body composition
Recent developments have led to the availability of several measurement techniques for assessing body composition including densitometry, dual energy absorptiometry (DEXA), tracer dilution techniques, neutron activation, ultrasound, magnetic resonance imaging (MRI), computerised tomography (CT) and bio-electric impedance analysis (BIA)3. Most of these techniques are complex, expensive and not practical for use in population studies and thus their use is restricted to research settings. A summary of these methods along with cost, ease of use, accuracy and effectiveness in assessing body fat is presented in Table 1.
Table 1. Methods of estimating body fat and its distribution

Anthropometric Measurements
Anthropometric measurements are often used, particularly in epidemiologic studies, as indirect methods to estimate the size of fat mass. The most commonly used of these measurements are stature (height), weight and skinfold thickness measurements.
Weight and height
Weight and height are simple and direct measures of body size that are easy to obtain in a variety of settings using relatively inexpensive instruments. Weight is highly correlated with body fat, but it also correlates with height, which is poorly associated with body fat. Thus weight adjusted for height is more useful than weight alone as an indicator of overweight4. There are two types of weight /height ratios: relative weight and power type indices.
Relative weight
Relative weight or weight for height is a common measure of overweight in children. It expresses the weight of a given subject as a percentage of the average weight of people of the same height and requires the use of tables of expected weight for the child’s height and sex5.
Power type weight and height indices
In addition to the height and weight tables, several indices have been proposed that relate weight to the n power of height (wt/ht(n)), such as the ponderal index (ht/wt –1/3), Rohrer index (wt/ ht3), Benn’s index (wt/ htp) and the Quetelet index or the body mass index (wt/ht2).
Body mass index (BMI)
The body mass index (BMI) is one of the most commonly used weight for height measures. It can be simply calculated by dividing the body weight in kilograms by the height in meters square (kg/m2). BMI offers a reliable and valid measure of obesity both in adults6 and in children and adolescents7,8,9 and is often employed in large-scale nutritional and epidemiologic studies. Although more reliably quantifiable than skinfold thickness, BMI measurements may be affected by variability in body frame size. It has been suggested that, in children, factors such as growth and development may complicate the use of BMI10. More recently however, BMI has been recommended as the most acceptable measure of body fat in children and adolescents which is both valid and reproducible as well as being easy to use11,12. In normal children, BMI increases slightly with age, thus BMI percentiles, which are age specific, are used to define risk categories.
Skinfold thickness
Total body fat can be predicted from skinfold thickness at various anatomical sites of the body, both in children and adolescents13. The most common sites used to assess children and adolescence adiposity are the subscapular skinfold measurement, which determines truncal body fat and the triceps skinfold, which measures fat in the extremities. Several prediction equations for assessing fat mass from skinfold measurement have been developed and cross-validated with other techniques for measuring body fat14,15. The clinical validity of skinfold measurement is well established. Triceps skinfold correlates positively with arteriosclerosis index and systolic blood pressure, and negatively with high-density lipoprotein cholesterol16.
Skinfold thickness measurement is simple and relatively inexpensive. However, there is growing concern regarding the comparability of the skinfold measurement across surveys and longitudinal studies, which monitor trends over time17,18. Reliability is often difficult to establish either for a single observer on the same subject or for different observers and it tends to decrease as body fat increases. In addition, the need to partially undress may not make this method culturally acceptable in some parts of the world. It may also lead to greater subject refusal and consequently bias4.
Waist circumference and waist –hip circumference ratio
Waist–hip circumference ratio is a well-recognised measure of regional fat distribution in the body and is often used as a marker for intra-abdominal fat accumulation. In adults there are gender differences in accumulation of intra-abdominal fat, which appears to be independent of the total amount of body fat19. Males often show a central or android pattern of fat distribution, whereas in females, body fat tends to accumulate in the thighs and buttocks resulting in a peripheral or gynaecoid pattern of adiposity. In men and women an increased WHR (>1.0 for males and >0.8 for females) is associated with greater risk of chronic diseases such as hypertension, stroke and ischemic heart disease2, 20 independent of total body fat 21. In children and adolescents, excessive intra-abdominal fat accumulation is associated with cardiovascular risk factors. Caprio et al22 have demonstrated a positive correlation between visceral fat mass and triglycerides and inverse relationship with high-density lipoprotein cholesterol in obese adolescent girls.
In adults both waist–hip ratio and waist circumference have been shown to be significantly associated with intra-abdominal fat23. Recent evidence suggests that waist circumference is the most preferred single anthropometric measurement for assessment of visceral adipose tissue24,25. Waist girth is easy to measure and correlates well with BMI, intra-abdominal fat mass and cardiovascular risk factors. Furthermore, reduction of waist circumference during weight loss in women has been shown to result in reduction in risks to cardiovascular diseases26.
In children and adolescents however, no correlation has been established between these measurements and intra-abdominal adipose tissue27,28. Using MRI to assess peripheral and intra-abdominal adipose tissue in obese and non-obese 10-15-year-old children, Brambilla et al29 showed that adiposity in children has a subcutaneous pattern and that there is no difference between sexes.
Individual trunk skinfold thicknesses and ratio of trunk to extremity skinfold thickness or circumference appear to be more important indicators of intra-abdominal adiposity in children and adolescents than waist-hip ratio. Fox et al28 used MRI to examine abdominal fat deposition in a group of 11-year-old children. Results showed that in girls sub-scapular skinfold thickness and waist circumference correlate well with intra-abdominal fat (r=0.8, r=0.76 respectively). Brambilla et al29 found that intra-abdominal fat in adolescents has a positive correlation with several trunk/ extremities such as waist/ arm and waist/thigh ratios and that in boys the sub-scapular/triceps skinfold ratio was the most important anthropometric measure of intra-abdominal fat(r=0.6).
Classification of obesity in children and adolescents
Obesity in children and adolescents is difficult to classify based on outcome criteria similar to those used for adults. Although adiposity in youth has been shown to be associated with adult morbidity and mortality30-32, available data are currently insufficient to support the development of a risk factor-based classification system for obesity in youth4. Thus a statistical approach is used in which obesity and overweight are defined relative to a selected percentile of a reference population based on age, sex and race-ethnicity33. These percentiles may be applied to a variety of anthropometric measures including skinfolds, weight for height and BMI.
Traditionally, obesity in children has been defined as a weight for height above the 90th percentile on the growth charts from the National Center of Health Statistics (NCHS), or weight in excess of 120 percent of the median weight for a given height. Super-obesity is defined as a weight for height above the 95th percentile and weight in excess of 140 percent of the median weight for a given height.
A recent workshop on childhood obesity convened by the International Obesity Task Force agreed to select BMI as an internationally acceptable index to assess adiposity in children and adolescents worldwide12. Cut-off points consistent with the internationally accepted cut-off points for adults’ morbidity of 25-30 have been proposed. Overweight was defined as a BMI value above the 80th percentile while a value greater than the 95th percentile was indicative of obesity. More recently, Cole et al34 have proposed age and sex specific cut off points for overweight and obesity in children which are linked to the adult obesity cut off points of 25 and 30 and based on pooled data from six large nationally representative surveys conducted in Brazil, Great Britain, Hong Kong, the Netherlands, Singapore and the United States.
Table 2.
Recommended cut off-values of body mass index and skinfold thickness for
adolescents
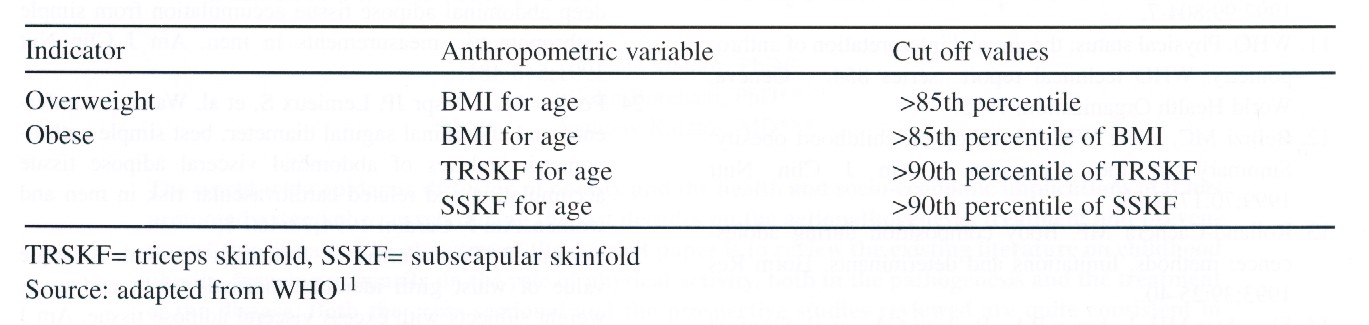
The World
Health Organisation expert committee, on the other hand, has recommended
the use of weight for height tables for determining overweight in children
and infants in populations11. A cut-off of > +2 Z score is considered to
be indicative of overweight in children. In case of adolescents, the WHO
expert committee has recommended the use of both the BMI for age and the
skinfold for age as the best indicators for the assessment of obesity in
this group. Overweight is defined as >85th percentile of BMI for
age while cut-off >85th percentile of BMI for age plus a >90th
percentile of triceps skinfold for age and a >90th percentile of
sub-scapular skinfold for age would be indicative of adolescent obesity.
Several countries have published BMI for age charts for their population
as well as defined cut-off points for overweight and obesity. Table 2 shows
indices and cut-off points used in different countries to define obesity
in children. The WHO has suggested that in the absence of local reference
data, the United States’ BMI for age data, as published by Must et al35
should be used. (Table 2).
CONCLUSION
There are several methods for measuring obesity in various ages and sexes. Each method has its advantages and disadvantages. However, the selection of these methods depend on many factors such as the cost, accuracy, ease of use, facilities and availability of trained personnel. In the Arab Gulf countries, most studies have used body mass index and skinfold thickness to determine overweight and obesity. These measurements are easy to obtain and some of them (body mass index) have a relatively good level of accuracy. Measurements may be difficult to use at this time, mainly due to the absence of facilities to carry out such measurements.
REFERENCES
1. Seidell
JC, Durenberg P, Hautvast JGA. Obesity and fat distribution in relation
to
health. Current insights and recommendations. World Review
of Nutrition and
Diet 1987;50:57-91.
2. WHO. Obesity:
preventing and managing the global epidemic. Report of a WHO
consultation on obesity. Geneva: World Health Organisation, 1998.
3. Harsha
D, Bray G. Body composition and childhood obesity. Endocrinology
and
Metabolism. Clinics of North America 1996;25:871-85.
4. Power C,
Lake JK, Cole TJ. Measurement and long-term health risks of child
and
adolescent fatness. Int J Obes 1997; 21:507-26.
5. Gibson
RS. Principles of Nutritional Assessment. Oxford University Press, New
York, 1990.
6. Garrow
JS, Webester J. Quetlet index (W/Ht)2 as a measure of fatness. Int
J obes
1985;9:147-53.
7. Rolland-Cachera
MF, Bellisle F, Deheeger M, et al. Influence of fat distribution
in adulthood: A two-decade follow-up study. Int J Obes 1990;14:473-81.
8. Pietrobelli
A, Faith MS, Allison, DB, et al. Body mass index as a measure of
obesity in children and adolescents. A validation study. J Pediat
1998;132:204-
10.
9. Malina
RM, Katzmarzyk PT. Validity of the body mass index as an indicator
of
the risk and presence of overweight in adolescents. Am J Clin Nutr
1999;70:131S-6S.
10.
Daniels SR, Khoury PR, Morrison JA. The utility of body mass index as a
measure of fatness in children and adolescents. Difference by race and
gender.
Pediatrics 1997;99:804-7.
11.
WHO. Physical status: the use and interpretation of anthropometry. WHO
technical report series 854. Geneva: World Health Organization,
1995.
12.
Bellizi MC, Dietz WH. Workshop on childhood obesity: Summary of the
discussion. Am J Clin Nutr 1999;70:173S-5S.
13.
Rolland-Cachera MF. Body composition during adolescence: methods,
limitations and determinants. Horm Res 1993;39:25-40.
14.
Slaughter MH, Lohman RA, Boileau CA, et al. Skinfold equation
for estimation
of body fatness in children and youth. Human Biology 1988;60:709-23.
15.
Goran MI, Driscoll P, Johnson R, et al. Cross calibration of body
composition
techniques against dual energy X ray absorptiometry in young children.
Am J
Clin Nutr 1996;63:299-305.
16.
Kanda A, Watanabe Y, Kawaguchi T. Estimation of obesity in school
children
by measuring skinfold thickness. Public Health 1997;111:29-32.
17.
Himes JH. Reliability of anthropometric methods and replicate measurements.
Am J Anthropol 1989;79:77-80.
18.
Chumlea WC, Guo S, Kuczymarski RJ, et al. Reliability for anthropometric
measurements in the Hispanic, Health and Nutrition Examination survey
(NHANES 1982-1984). Am J Clin Nutr 1990;51:902S-7S.
19.
Lemieux S, Prudhomme D, Bouchard C, et al. Sex differences in relation
to total
body fatness. Am J Clin Nutr 1993;58:463-7.
20. Larsson
B, Svardsudd K, Welin L, et al. Abdominal adipose tissue distribution,
obesity and risk of cardiovascular disease and death: 13 year follow up
of
participants in the study of men born in 1913. Br Med J 1984;288:1401-4.
21.
Bjorntorp P. Abdominal fat distribution and disease: an overview of
epidemiological data. Ann Med 1992;24:15-8.
22.
Caprio S, Hyman L, McCarthy S, et al. Fat distribution and cardiovascular
risk
factors in obese adolescent girls. Am J Clin Nut 1996;64:12-7.
23.
Despr JP, Prudhomme D, Pouliot MC, et al. Estimation of deep
abdominal
adipose tissue accumulation from simple anthropometric measurements in
men.
Am J Clin Nut 1991;548-481.
24.
Pouliot MC, Despr JP, Lemieux S, et al. Waist circumference and abdominal
sagittal diameter: best simple anthropometric indexes of abdominal visceral
adipose tissue accumulation and related cardiovascular risk in men and
women.
Am J Cardiol 1994;73:460-8.
25.
Lemeux S, Prudhomene D, Bouchard C, et al. A single value of waist girth
identifies normal-weight and overweight subjects with excess visceral adipose
tissue. Am J Clin Nutr 1996;64:685-93.
26.
Han T, Richmond P, Avenell A, et al. Waist circumference reduction and
cardiovascular benefits during weight loss in women. Int J Obes 1997;21:127-34.
27.
De Ridder CM, de Boer RW, Seidell JC, et al. Body fat
distribution in pubertal
girls quantified by magnetic resonance imaging. Int J Obes 1992;16:443-9.
28.
Fox K, Peters D, Armstrong N, et al. Abdominal Fat deposition in
11 year old
children. Int J Obes 1993;17:6-11.
29.
Brambilla P, Manzoni P, Sironi S, et al. Peripheral and abdominal
adiposity in
childhood obesity. Int J of Obes 1994;18:795-800.
30.
Must A, Jacques PE, Dallal GE, et al. Long- term morbidity and mortality
of
overweight adolescents, a follow up of the Harvard Growth Study of 1922
to
1985. N Engl J Med 1992;327:1350-5.
31.
Must A. Morbidity and Mortality associated with elevated body weight in
children and adolescents. Am J Clin Nut 1996;63:445S-7S.
32.
Toriano RP, Flegal KM. Overweight children and adolescents: Description,
epidemiology and demographics. Pediatrics 1998;101:525-39.
33.
Cole TJ, Bellizi M, Flegal K, et al. Establishing a standard definition
for child
overweight and obesity worldwide: international survey. Br Med J
2000;320:1240-3.
34.
Must A, Dallal GE, Dietz WH. Reference data for obesity: 85th
and 95th
percentile body mass index (wt/ht2) and triceps skinfold thickness. Am
J Clin
Nutr 1991;53:839-46.

Copyright 2000, Bahrain Medical Bulletin