Coronary heart disease includes a number of interdependent syndromes: angina pectoris, acute myocardial infarction, and sudden cardiac death (due to lethal arrhythmias). There are also features of coronary occlusion (blockage of a coronary artery), including phasic abnormalities during rest and exercise electrocardiograms that indicate the presence of myocardial ischemia.
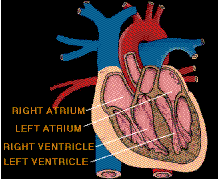
Coronary arteries of the heart
Epidemiology.
There is an uneven geographic distribution of coronary heart disease. It is responsible for
one-third to one-half of the deaths in most industrialized countries and is the most common single
cause of death in North America and Europe.
Ischaemic heart disease is also one of the leading causes of death in Malaysia. Many studies have linked the geographic differences in coronary heart disease with various aspects of life-style, such as cigarette smoking, diet, physical inactivity, and obesity.
Pathology
Ischaemic heart disease is due to partial or total blockade of coronary arteries, leading to various
syndrome like angina, infarct or sudden death.
The blockade of artery is a result of formation of artheroma plaque in the arterial wall. This process is known as artherosclerosis. It results in narrowing of the arterial lumen. When this is complicated by thrombosis (blood clot), the whole artery is blocked and causes a myocardial infarction.
It is impossible to incriminate any one of these risk factors over another, since the manifestations of coronary heart disease are undoubtedly due to many independent and interdependent influences, but the coexistence of the three greatly increases the risk of developing coronary heart disease.
The familial predisposition to the disease is not well understood, although it is stronger in families with hypercholesterolemia and hypertension. It is most likely to develop prematurely in the presence of polygenic forms, or the rare monogenic form, of familial hypercholesterolemia. There is a progressive relationship between serum cholesterol concentrations and the incidence of coronary heart disease. This is also true for hypertension.
Of the three major risk factors, however, excessive cigarette smoking is probably the most important. Other influences--such as a predisposition to develop thrombosis, diabetes mellitus, physical inactivity, obesity, and, rarely, oral contraceptives--may induce premature coronary heart disease in susceptible persons.
Angina pectoris
.
There are no truly characteristic symptoms
of angina pectoris. While the chest discomfort may be variously described as "constricting,"
"suffocating," "crushing," "heavy," or "squeezing," there are many patients in whom the quality of
the sensation is imprecise. The discomfort is usually, but not always, behind the breastbone, but
pain radiating to the throat or jaw or down the inner sides of either arm is common. There may be
no physical abnormalities, and an electrocardiogram may be normal or show only transient
changes with exercise.
Coronary arteriography assesses the extent of coronary artery occlusion, which may vary from a small increase in coronary artery muscle tone at a partly occluded site in a branch of one of the three main coronary arteries, to a 90 percent or greater occlusion of the left main coronary artery with involvement of other major coronary arteries.
The myocardial ischemia that causes angina is due to a disturbance of the balance between myocardial demands and supply. If demands are reduced sufficiently, the temporarily endangered supply may be adequate. The disturbance of the equilibrium may be short-lived and may correct itself. Unstable angina has an appreciably worse prognosis than stable angina because of a higher risk of myocardial infarction and sudden cardiac death, and it requires daily observation and active intervention.
When coronary arteriography reveals relatively isolated, incompletely obstructive lesions, there are two alternative treatments--medication or coronary angioplasty (balloon dilation of the localized obstruction by a special catheter).
In unstable angina pectoris, coronary arteriography may help determine whether coronary angioplasty or coronary artery bypass surgery is needed. Drugs that cause coronary dilation and peripheral arterial vasodilation, and that reduce the load on the heart, are usually necessary. Drugs that reduce the work of the heart by blocking adrenoreceptors (receptors in the heart that respond to epinephrine) and drugs that reduce a thrombogenic tendency are given at this stage. For patients with stable angina, drugs that reduce the heart's work are administered.
Myocardial infarction.
A syndrome of prolonged, severe chest pain was first described in the medical literature in 1912
by James Brian Herrick, who attributed the syndrome to coronary thrombosis, the development
of a clot in a major blood vessel serving the heart. As a result, the disorder was termed coronary
thrombosis, or coronary occlusion (blockage of a coronary artery).
Later evidence indicated, however, that, though thrombotic occlusion of an atheromatous lesion in a coronary artery is the most common cause of the disorder, the manifestations are the result of the death of an area of heart muscle (infarction). The term myocardial infarction, therefore, is more appropriate. The more general and less specific term heart attack may be more desirable because of these difficulties in describing the causation of the disease entity.
Myocardial infarction is characterized by cellular death (necrosis) of a segment of the heart muscle. Generally, it involves an area in the forward wall of the heart related to the blood distribution of the anterior descending coronary artery, though in other instances the inferior wall or the septum (partition) of the ventricle is involved. Coronary thrombosis is present in a majority of the hearts examined at autopsy and undoubtedly plays an important role. In others, changes in metabolic demands of the heart muscle in the presence of a restricted blood flow may be enough to cause death of ischemic cells.
The outstanding clinical feature of myocardial infarction is pain, similar in many respects to that of angina pectoris. The important difference is that the pain lasts for a much longer period, at least half an hour, and usually for several hours and perhaps for days.
The pain is described as "crushing," "compressing," "like a vise," and is often associated with some difficulty in breathing. As with angina pectoris, the pain may radiate to the left arm or up the neck into the jaws.
There is often nausea, vomiting, and weakness. Fainting (syncope) may occur. The affected person frequently is pale, and he may perspire profusely.
Infrequently, these symptoms may be absent, and the occurrence of infarction can then be detected only by laboratory tests. Laboratory studies may show an elevation of the number of white blood cells in the blood or a rise in the enzyme content of the blood, indicating leakage from damaged heart muscle cells.
The electrocardiogram in most instances shows distinct and characteristic abnormalities at the onset, but the electrocardiographic abnormalities may be less characteristic or totally absent.
In most persons who experience an acute myocardial infarction, the circulation remains adequate. In a small percentage of cases, the state of shock occurs, with pallor, coolness of the hands and feet, low blood pressure, and rapid heart action. In these cases, myocardial infarction is deadly, with survival rates of only 20-40 percent, in contrast to the current survival rate in many hospitals of 80-90 percent.
Mortality is also related to age, for the process is more lethal in the elderly. In a small number of persons there may be thromboembolism (obstruction caused by a clot that has broken loose from its site of formation) into an artery elsewhere in the body.
Drugs are used to control arrhythmias and to strengthen myocardial function. Convalescence from an acute myocardial infarction may last several weeks, allowing time for scar tissue to form in the area of an infarction and a gradual return to activity. Although some persons may have residual evidence of heart failure or other cardiac malfunction, most individuals may return to an active life after a period of weeks and are not in any way invalided by the process. These individuals do, however, have an increased potential for subsequent myocardial infarction.
Sudden death.
The term sudden death is used imprecisely and includes death that is almost instantaneous as well
as death in which rapidly deteriorating disease processes may occupy as much as two or three
days. In heart disease both may occur, but the term characteristically refers to instantaneous
death, which is frequent in coronary heart disease. Sudden death from coronary heart disease
occurs so frequently that less than half of the persons who die from heart attacks each year in the
United States survive long enough to reach the hospital.
Instantaneous cardiac death is usually due to ventricular fibrillation (an uncontrolled and uncoordinated twitching of the ventricle muscle), with total mechanical inadequacy of the heart and erratic and ineffective electrical activity. Sudden death may occur without any previous manifestations of coronary heart disease. It may occur in the course of angina pectoris and causes about one-half of the deaths due to acute myocardial infarction in hospitalized patients, though this number is decreasing with the more widespread use of coronary-care units. Although a reduced supply of blood to the heart undoubtedly is the precipitating factor, acute myocardial infarction does not always occur. In most persons who have died almost instantaneously, no infarction was present, but there was widespread coronary artery disease. In rare instances, sudden death occurs without a major degree of coronary artery disease.
The use of closed-chest cardiopulmonary massage (massage of heart and lungs without making an opening in the chest wall), coupled with electrical defibrillation (the use of electrical shocks), if applied within a few minutes of the sudden death episode, may successfully resuscitate the majority of patients. In coronary-care units where the facilities and trained personnel are immediately available, the percentage of successful resuscitations is high. In general hospitals where resuscitation teams have been established, the percentage is less satisfactory. Sudden death outside the hospital is, of course, a more difficult problem, but mobile coronary-care units responding as emergency ambulances to the site of a sudden death are being used widely and successfully. Effective resuscitation depends upon the prompt arrival of the unit. The use of drugs and other means to prevent the onset of sudden death has been relatively successful in the coronary-care unit, except in situations in which the disease has been present for a long period of time.
Survival during and after a heart attack.
The risk of death from an arrhythmia is greatest within the first few minutes of the onset of an
occlusion in a coronary artery or of acute ischemia occurring in the region of the myocardium.
Thus, of those likely to die during the first two weeks after a major heart attack, 40 percent will
die within one hour of the onset and another 20 percent within the next three hours.
During the first few hours most persons have some disturbances of rhythm and conduction. Ventricular fibrillation is particularly common in the first two hours, and its incidence decreases rapidly during the next 10 to 12 hours. If undetected, ventricular fibrillation is lethal. It can be reversed, however, in 80 to 90 percent of patients with the use of appropriate electronic devices for monitoring heart rhythm, for giving a direct-current shock to stop it, and for resuscitation.
Both the immediate and long-term outlook of persons after myocardial infarction depends on the extent of myocardial damage and the influence of this damage on cardiac function. Efforts to limit or reduce the size of the infarct have been unsuccessful in improving the short- or long-term outlook. Procedures that cause thrombi to dissolve (thrombolysis), however, have led to the dramatic and immediate opening of apparently occluded coronary arteries. When such measures are implemented within four hours (and preferably one hour) of the onset of the heart attack, the chances of survival are greater, although it has not been shown that long-term prognosis is improved. Naturally occurring lytic enzymes (such as streptokinase) or genetically engineered products are used.
Coronary artery bypass surgery.
Coronary artery bypass surgery is widely used to restore adequate blood flow to the heart muscle
beyond severe atheromatous obstruction in the main coronary arteries. The most common
operation is one in which lengths of superficial veins are taken from the legs and inserted between
the aorta, usually above the sinuses of Valsalva, and joined to a part of a coronary artery below
the obstructive atheromatous lesion. Multiple grafts are often used for multiple atheromatous
occlusions. The internal mammary arteries are also used to provide a new blood supply beyond
the point of arterial obstruction; however, since there are only two internal mammary arteries, their
use is limited.
There are two principal uses for coronary artery bypass surgery. One is to relieve chest angina that is resistant to medication. The other is to prolong a person's life; however, this is only achieved when all three main coronary arteries are severely obstructed and when the contractility of the left ventricle has been impaired somewhat. Coronary artery bypass surgery does not prolong life when it is used to overcome an obstruction in only one or even two arteries.
Angioplasty.
The development of catheters with strong inflatable balloons constructed toward their end
and along the line of the catheter has greatly changed cardiac surgery. The balloons can be inflated
by compressed air at different controlled pressures. They are used for dilation of a partly
obstructed coronary artery (percutaneous transluminal coronary angioplasty, or PTCA), with
restoration of blood flow to the heart muscle, and of a severely obstructed heart valve, particularly
the aortic valve, relieving the pressure on the left ventricle.
The procedure generally requires no anesthetic and, using specialized radiological imaging techniques, is sometimes done on an outpatient basis. Several coronary arteries may be dilated in this way, with flattening of the atheromatous material against and into the arterial wall. Although there are operative risks, such as emboli and tearing, the results are excellent and the technique may be repeated, if necessary.
Heart transplantation.
If the heart muscle has been damaged beyond surgical repair, heart transplantation may be
performed. The diseased heart is removed and the donor's heart is sewn in position. This
procedure is particularly useful in advanced cardiomyopathy. Half of all heart transplant patients
survive five years after the surgery. Heart-lung transplants are used for some intractable
cardiopulmonary diseases, such as cystic fibrosis. The success rates of both of these operations
has grown.
Artificial heart.
Many scientists are directing their efforts toward development of an artificial heart. The
heart-lung machine effectively supports the circulation for a few hours; if it is used for longer
periods, the blood is damaged by the pumping and oxygenation. Current research is directed
toward development of pumps and oxygenators that can be used for partial or total support of the
circulation for long periods without damage to the blood.

Partial cardiac assistors have been used successfully to aid the heart after operation until it has had sufficient time to recover. One of these is the left ventricular bypass pump. It reduces the work load of the heart because blood is removed from the left atrium of the heart and pumped back to the body through the axillary artery. No oxygenator is required because the lungs are not bypassed. (M.E.DeB./ E.B.D./M.F.O.)
Prevention of coronary heart disease.
Most physicians recommend the elimination of cigarette smoking, a reduction of dietary saturated
fat, a proportional increase in fat calories from polyunsaturated sources, a reduction in high blood
pressure, an increase in physical activity, and the maintenance of a weight within normal limits.
While the circumstantial evidence from many kinds of studies supporting these measures is
impressive, they have not yet been shown to be as effective as expected or predicted. While
claims are made that a decrease in the rate of death from heart disease in the United States,
Australia, Finland, and other countries is due to such changes in life style, similar changes in life
style elsewhere have not been associated with a decrease in the death rate. In some countries
(such as Sweden) coronary mortality has actually risen. Those persons, however, who come from
high-risk families, such as those with familial hypercholesterolemia, have benefited from reduction
of high levels of serum cholesterol. - Mosby Medical Encyclopaedia, Ency. Britannica
 HOME
HOME